Introduction
Acute cerebral venous thrombosis (CVT) is a rare condition, which comprises 0.5-1% of all strokes [1,2]. It affects cerebral veins and dural sinuses of both the superficial and deep venous systems. Cerebral venous thrombosis may cause brain swelling, local venous oedema, or infarction, which is very often haemorrhagic. Clinical symptoms are very often non-specific with severe headache, seizure, confusion, and loss of consciousness being the most common findings. In some cases, it can lead to a serious clinical state that may progress to coma or even death, thus prompt diagnosis and treatment are mandatory. Cerebral venous thrombosis occurs more commonly in patients with certain risk factors, such as intake of oral contraceptives, pregnancy, steroid treatment, prothrombotic state, skull trauma, infections especially mastoid sinusitis, sepsis, malignancy, connective tissue disorders, or dehydration [3]. Nowadays, due to the COVID-19 pandemic situation, this topic has become particularly relevant. The viral infection itself or even complications after AstraZeneca vaccination can also cause CVT by mechanisms of vaccine-induced thrombosis and thrombocytopaenia (VITT) [4].
Because patients with CVT usually develop acute neurological symptoms, the first imaging modality is computed tomography (CT) of the brain in an emergency department. It must be stressed that due to non-specific clinical symptoms, neuroimaging plays a crucial role in the initial prompt diagnosis. Emergency CT is usually performed without contrast administration [5,6] and may show hyperdense thrombi within cerebral veins or dural sinuses as well as findings secondary to venous congestion such as generalized brain swelling, areas of hypodense local oedema, or venous haemorrhagic infarctions [5]. Computed tomography with iodine contrast injection is sometimes used in emergency settings and may show filling defects within thrombosed veins or dural sinuses, gyral enhancement, or prominent intramedullary veins [5]. The gold standard in the diagnosis of CVT is the use of venographies with contrast injection, such as CT venography, magnetic resonance (MR) venography, or conventional digital subtracted angiography (DSA), which are the best examinations for the assessment of morphology and patency of dural sinuses and veins. Magnetic resonance venography may be performed with or without contrast administration, but the latter has low specificity and many false positive results [1]. Magnetic resonance venography is a part of the MR examination, and other sequences such as T1- and T2-weighted images, FLAIR, diffusion-weighted imaging (DWI), susceptibility-weighted imaging (SWI), and postcontrast T1-weighted images are very helpful in the diagnosis of CVT and its complications, but MRI is rarely used in emergency settings.
It must be emphasized again that the initial diagnosis of CVT is usually based on emergency CT examinations performed without or with contrast injection, and interpretation of these studies may be very challenging. Despite the growing knowledge of this disease, the diagnosis of CVT is often delayed and thus the therapy is not implemented at the right time. In one study an average delay of 7 days between the onset of the symptoms and imaging-based diagnosis was found [1]. Pitfalls and misinterpretations of CT studies in CVT are not a new topic in the literature, but it must be stressed that it is still a serious problem for radiologists to diagnose it correctly during emergency reporting sessions, and a delay in the correct diagnosis may have serious consequences to patients. We believe that the awareness of this disease, its diversity and severity, as well as pitfalls in interpretation of brain CT are mandatory for medical staff working in emergency departments, especially radiologists reporting difficult images under pressure of time and very often late at night when the risk of mistakes is even higher. The diagnosis of CVT requires cooperation between radiologists and other clinicians because both imaging and clinical symptoms may be non-specific and misleading.
The purpose of this study was to retrospectively analyse emergency brain CT examinations in CVT cases performed in an academic centre to assess the rate of misdiagnosed cases and to analyse the major pitfalls in the interpretation of lesions within both vessels and brain parenchyma in order to raise awareness of the problem in groups of radiologists and clinicians and to decrease the still high level of incorrect or delayed diagnoses of acute CVT.
Material and methods
The material consisted of 31 emergency CT examinations of the brain performed in the period 2015-2019 in the Emergency Department at Wroclaw University Hospital, which were retrospectively analysed for signs of CVT. The CT studies were chosen from the large database of emergency head CT examinations, and only those with the diagnosis of CVT confirmed in follow-up examinations such as CT venography, MRI with contrast administration, or DSA were included in the study. The CT technique included thin-slice volume acquisition, which was reformatted into alternative planes for further analysis. The final study group consisted of 22 CT examinations without contrast administration and 9 CT examinations with contrast injection, which were retrospectively analysed in regard to signs of CVT both within the cerebral venous system and brain parenchyma. In the correct diagnosis group 4 of the CTs were reported by certified neuroradiologists and 11 by general radiologists. In the incorrect diagnosis group all of the 16 CTs were reported by general radiologists.
The final study group contained 19 women and 12 men (mean age: 42.6 years, range: 4-94 years). Acute clinical symptoms were mostly headache and seizures, followed by hemiparesis and loss of consciousness. The CVT causes and risk factors were as follows: oral contraceptives, hormonal infertility treatment, caesarean section, middle ear infection with mastoiditis, nephrotic syndrome, advanced malignant disease, and temporal bone fracture. In some cases the causes were not known.
Results
Retrospective analysis of all 31 emergency CT examinations showed thrombosed dural sinuses in 24/31 (77.4%) cases, thrombosed veins in 7/31 (22.6%) cases, and no lesions within vessels in 2/31 (6.5%) cases. Haemorrhagic lesions were found in 9/31 (29%) cases, hypodense oedema in 6/31 (19.6%) cases, brain swelling in 1/31 (3.2%) cases, and no parenchymal lesions were revealed in 15/31 (48.4%) cases.
Retrospective analysis of 31 emergency CT examinations showed 2 groups of patients: with a correct diagnosis of CVT established in 15 cases (48.4%) and with an incorrect diagnosis in 16 cases (51.6%) (Tables 1 and 2).
Table 1
Results of computed tomography (CT) evaluation of the patients with the correct diagnosis of cerebral venous thrombosis in the emergency CT studies
Table 2
Results of computed tomography (CT) evaluation of the patients with incorrect interpretation of the emergency CT studies
In the first group of patients with a correct diagnosis of CVT, 10 CT examinations were performed without contrast injection and 5 CT studies with contrast administration. All 15 cases showed signs of venous thrombosis within vessels, 6 cases (40%) had additional parenchymal lesions (haemorrhagic in 3 cases and non-haemorrhagic in 3 cases), while in 9 cases (60%) there were no brain lesions found in the retrospective analysis. Diagnosis of deep venous thrombosis was made in 1 case (6.65%), superficial venous thrombosis in 13 cases (86.7%), and complex venous thrombosis of deep and superficial venous systems in 1 case (6.65%) (Table 1).
In the second group the diagnosis of CVT was delayed due to an incorrect interpretation of CT examinations performed at the emergency department, and the correct diagnosis was established in the follow-up examinations. In these cases, 12 emergency CT studies were performed without contrast injection and 4 examinations with contrast administration. Deep venous thrombosis was diagnosed in 1 case (5.6%) while superficial venous thrombosis in 15 cases (94.4%). Complex venous thrombosis of the deep and superficial venous systems was not observed (Table 2).
Retrospective analysis of 16 incorrectly interpreted CT examinations showed 4 groups of subjects: 1 – with both vascular and parenchymal lesions, which were overlooked (8/16 cases, 50%), 2 – with vascular lesions only, which were either overlooked, misinterpreted, or covered by artefacts (5/16 cases, 31.3%,), 3 – with parenchymal lesions only, which were misinterpreted (2/16 cases, 12.5%), and 4 – with no lesions present in the emergency head CT (1 case, 6.2%) (Table 2). Overlooked brain lesions were areas of non-haemorrhagic oedema in 2 cases while a large number of brain lesions were misinterpreted: nonhaemorrhagic lesions as low-grade tumours (2 cases) and 6 haemorrhagic cases as equivocal lesions (contusion or of unknown vascular origin) in 3 cases, as brain contusions in 2 cases and as metastases in 1 case (Table 3). Vascular pathologies that were most often overlooked included thrombosed sigmoid sinuses in 4 cases, cortical veins in 4 cases, straight sinus in 2 cases, and superior sagittal sinus, transverse sinus, and deep veins in 1 case each (Table 3). Figures 1, 2, and 3 show the examples of overlooked or misinterpreted vascular and parenchymal pathology in the course of CVT.
Figure 1
Cases of cerebral venous thrombosis that were reported as normal due to overlooking the thrombosed hyperdense vessels (arrows) such as the anterior aspect of the superior sagittal sinus (A), straight sinus (B), right cortical vein (C), and the left transverse sinus (D)
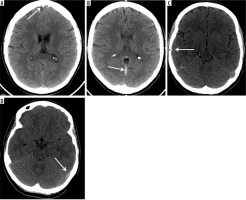
Figure 2
Cases of haemorrhagic infarctions due to cerebral venous thrombosis reported as other haemorrhagic lesions such as brain contusion (A) or vascular lesion of uncertain aetiology (B) because of the absence of hyperdense thrombosed venous vessels on emergency computed tomography images. Note a very characteristic pattern of multiple ovoid haemorrhagic lesions surrounded by hypodense oedema in the cortical-subcortical location that should always raise a suspicion of bleeding during cerebral venous thrombosis
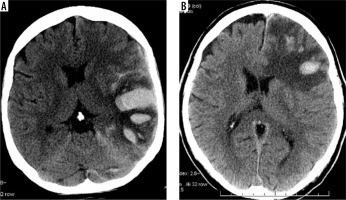
Figure 3
Cases of brain lesions during cerebral venous thrombosis (short arrows) that were reported as other pathologies due to overlooking the thrombosed vessels (long arrows) such as right transverse sinus (A), bilateral cortical veins (B), and posterior aspects of the superior sagittal sinuses (C, D). Hypodense cortical oedema in the right temporal lobe was reported as low-grade glioma (A) while haemorrhagic venous infarctions were reported as haemorrhagic metastases (B), unequivocal vascular lesion (C), and brain contusion (D)
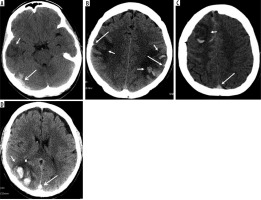
Table 3
Reasons for the incorrect diagnosis of cerebral venous thrombosis (CVT) in the emergency computed tomography examinations
Discussion
The purpose of the study was to retrospectively analyse emergency CT examinations in CVT cases to assess the rate of misdiagnosed cases and analyse major pitfalls in the interpretation of both vessel and cerebral pathology. The study was performed in the university hospital, which employs experienced radiologists working in the emergency department.
In CVT typical radiological findings on non-contrast CT scans are hyperdensity of dural sinuses (dense dural sinus sign) and hyperdense deep or cortical veins (the latter referred as the cord sign), while filling defects within contrasted dural sinuses or veins may be seen on enhanced CT studies [1]. According to some reports hyperdense thrombosed sinuses are visible only in 25% and thrombosed veins in 5-20% of CVT cases [7-9]. More recent studies, however, indicate that plain CT is very sensitive in the detection of CTV [8].
Our retrospective analysis of 31 emergency CT studies showed a higher incidence of thrombosed dural sinuses in 24/31 cases (77.4%) and hyperdense veins in 7/31 (22.6%) cases. It is worth stating that only 2/31 (6.5%) cases showed no hyperdensity within the venous system in the retrospective analysis. According to the literature, abnormalities in the brain are present in 40-60% of CVT cases, with parenchymal haemorrhage in 30-35% of cases typically in the cortex or cortical-subcortical location [10]. In our study haemorrhagic lesions were found in 9/31 (29%) cases, hypodense oedema in 6/31 (19.4%) cases, brain swelling in 1/31 (3.2%) cases, and no parenchymal lesions were revealed in 15/31 (48.4%) cases.
In our study retrospective analysis of the emergency CT examinations revealed that less than half of the CVT cases (48.4%) were correctly diagnosed. Other studies showed similar results, when the diagnosis was not suspected on clinical grounds, the false-negative rate on CT was reported as 53% [1]. In our study all 15 cases that were correctly diagnosed showed radiological features of thrombosis within dural sinuses or veins. It must be stressed that only 1/3 of these CT studies was performed with the contrast injection, which means that the thrombosed vessels were highly visible on non-enhanced CT images. In most of these cases no parenchymal lesions were found, so the correct diagnosis of CVT was made exclusively based on an adequate interpretation of hyperdense vessels.
Even more interesting results were obtained from the analysis of the incorrect diagnoses. Retrospective analysis revealed that an incorrect diagnosis was most often caused by misinterpretation or overlooking of parenchymal lesions or thrombosed veins and dural sinuses (Figures 1-3). In 6 cases brain haemorrhagic lesions due to CVT were misinterpreted as different pathologies such as brain contusions (2 cases), metastases (1 case), or haemorrhage of uncertain cause (3 cases). According to the literature the diagnosis of CVT is very challenging because it may mimic other pathologies, as was the case in our study. Other studies also reported that lesions due to CVT were misinterpreted; for example, thrombosed cortical veins as a subarachnoid haemorrhage or a subdural haematoma, focal brain haemorrhage as haemorrhagic contusions, and focal oedema or haemorrhage as brain tumours [11]. The authors concluded that it is essential to always correlate imaging findings with the clinical context and to look for other lesions, especially within dural sinuses and veins [12]. It must be stressed that haemorrhagic lesions are fairly typical for venous infarctions, and because the thrombosis of the superficial system is more common than the deep venous system they are usually located within the cortex or at the grey-white matter junction, as in our cases. Especially when the haemorrhage is located within the lateral aspect of temporal lobe – in draining territory of the vein of Labbe or parasagittal high convexity – the suspicion of CVT should be raised [9]. They also show quite typical morphology of single or multiple ovoid hyperdense foci (Figures 2 and 3) [8,13,14]. They are easy to see, so the main source of incorrect diagnoses of CVT in these cases is based on their misinterpretation as different pathologies. On the other hand, non-haemorrhagic parenchymal changes due to CVT may also be misinterpreted, but they may also be overlooked because they are often very subtle. In our study non-haemorrhagic brain lesions were misinterpreted as low-grade tumours or overlooked due to very mild hypodensity that was not noticed and the CT studies were reported as normal. Hypodense lesions due to CVT represent venous congestion and oedema, which are potentially reversible [9]. Misinterpretation of cerebral lesions due to CVT as brain tumours may have very serious consequences including unnecessary brain biopsies. One of our patients was prepared for a brain biopsy, which was finally cancelled after a review of CT and MR images with an experienced neuroradiologist.
Retrospective analysis of errors in the interpretation of changes within the venous system showed that they were mostly due to overlooking of the signs of thrombosis in dural sinuses or veins. The most commonly overlooked vessels were cortical veins (4 cases) and sigmoid sinus (4 cases), and less often straight sinus (2 cases) followed by the superior sagittal sinus, transverse sinus, and deep veins (1 case of each). According to the literature, the most commonly involved sinus is the superior sagittal sinus (63%), followed by the transverse sinus (57%), and then the sigmoid and straight sinuses (each 15%) [10].
Overlooking of hyperdense vessels is often due to a lack of appropriate attention to the appearance of dural sinuses and cortical veins (Figure 1). Nonetheless, the difficulty may also be caused by the location of dural sinus on the edges of an image, the end of the series of images, i.e. the superior sagittal sinus. Therefore, multiplanar reformats (MPRs) may help in avoiding errors of interpretation. Cortical veins are small vessels that are not easily seen, and spotting them requires active searching by a radiologist suspecting CVT. Thrombosed hyperdense dural sinuses or veins are misinterpreted less often than other pathologies. In our study, 2 cases of hyperdense sigmoid and transverse sinuses were misinterpreted as pericerebellar haematomas. Again, it is always crucial to correlate imaging findings with the clinical context. For example, whenever there is a pathology of the mastoid bone such as inflammation or fracture, CVT of the sigmoid sinus should be suspected in the first place rather than pericerebellar haematoma. It should be remembered that in some cases thrombosed vessels may be covered by artefacts, like in one of our cases in which a thrombosed sigmoid sinus was entirely obscured by artefacts and correctly diagnosed in a follow-up MR examination.
When analysing patients with incorrect diagnoses, we divided them into 4 groups: 1) patients with visible vascular and brain lesions, 2) patients with only vascular lesions present, 3) patients with only brain lesions present, and 4) patients with no visible changes within the brain parenchyma nor within vessels. Surprisingly, we found that 8/16 (50%) of the incorrectly reported cases belonged to the first group and the other 5/16 (31.2%) cases to the second group, which should be the easiest groups to be diagnosed. The third group of CVT patients with only brain lesions visible on CT included 2 cases in whom haemorrhagic lesions were misinterpreted as other pathologies (Figure 2). This kind of CVT manifestation with only parenchymal lesions present is very challenging because of the lack of any hint from the thrombosed hyperdense vessels. It must be remembered that suspicion of CVT should be raised, even in the absence of visible vessels, when haemorrhagic or non-haemorrhagic parenchymal lesions are present in the cortical location or at the grey-white matter junction (CVT of the superficial venous system) or bilaterally in the deep structures including thalamus and basal ganglia (CVT of the deep venous system) [7,8,15,16].
Finally, it must be stressed that radiological signs of CVT may be very subtle or even absent such as in the fourth group of our misdiagnosed patients. For that reason, in our study 4/16 cases (23.5%) were reported as normal. In 3 of them the retrospective analysis revealed single hyperdense thrombosed vessels or areas of a very subtle hypodense oedema, which were overlooked in the initial emergency report. These are especially challenging cases because the radiological signs are very subtle and easy to miss. The risk of mistake is even greater when we remember that radiologists interpreting those difficult studies work in emergency conditions, under pressure of time, or at night. What is even worse, patients with CVT may not develop any lesions visible in the emergency CT, as was found in 1 patient in our study (group 4). If neurological symptoms persist, a follow-up CT scan with contrast injection or, even better, MRI with contrast administration should be considered [7,8].
As we showed in our study the rate of the correct diagnoses of acute CVT based on the emergency CT studies is less than 50%, which is not satisfactory. The reasons for that are misinterpretation or overlooking of imaging symptoms by radiologists. It shows the need for constant training of radiologists, raising their awareness about this disease and its pitfalls. Finally, it must be stressed that there were differences in the rate of misdiagnoses between general radiologists and certified neuroradiologists. The latter correctly diagnosed all CVT cases, highlighting the importance of high-level expertise and proper training. Hopefully this review of our cases will be of benefit to the continued education of general radiologists, who are responsible for CT head reporting in most hospitals. On the other hand, in our opinion good cooperation between clinicians and radiologists working in emergency settings could also increase the rate of correct diagnoses of acute CVT. Appropriate information about clinical signs or clinical suspicion of CVT may influence the final radiological report, as was also emphasized in a paper by Tang et al. [1,17-19]. The authors of this study noted that suspicion of CVT was listed as the clinical diagnosis only in 5% of referrals for CT and in 33% referrals for MRI [16,20]. Although the symptoms of CVT are rather non-specific such as headache, seizures, loss of consciousness, or hemiparesis, the coexistence of other medical conditions such as oral contraceptives, hormonal infertility treatment, caesarean section, nephrotic syndrome, or advanced malignant disease should raise suspicion of CVT. Radiologists should also consider CVT always in cases of young women with headache or seizures, or whenever there is a pathology of the mastoid bone – either a fracture or an infection [16].
Conclusions
Acute CVT is still an underdiagnosed pathology in emergency head CT studies, with over 50% of incorrect diagnoses even in specialized university centres, leading to a suspicion that this rate could be even higher in other less specialized centres. In the majority of cases head CT without contrast injection is sufficient to make a correct diagnosis. The main sources of error are overlooking thrombosed hyperdense vessels (especially subtle changes within dural venous sinuses and small cortical veins) and misinterpretation of parenchymal brain lesions, especially haemorrhagic ones. We emphasize the role of a detailed analysis of the venous system on each unenhanced CT scan performed in the emergency settings together with knowledge about the typical distribution and morphology of parenchymal lesions in the course of CVT. We also strongly recommend good clinical-radiological cooperation in reaching a final, correct diagnosis, especially in young patients with headache or seizures and haemorrhagic brain lesions. We hope that this analysis will raise the awareness of CVT among emergency doctors, especially general radiologists and neurologists, and help to reduce the rate of delayed diagnoses of CVT, which may cause serious complications to patients. Feedback about mistakes made within a radiology department must be open and non-confrontational for the educational benefit of radiologists, which ultimately improves the care of patients. Radiologists should therefore always keep the diagnosis of CVT in mind whenever reporting emergency CT brain scans.






