Introduction
Trochlear dysplasia (TD) is characterized by modification in the shape of the femoral trochlear [1,2] and is most prevalent in female adolescents and young adults. The shape of a normal femoral trochlear is concave, allowing the patellar to sit in its usual position throughout the range of movement of the knee joint [1]. In TD, the trochlear is either flat or convex (in severe conditions), hindering the stability of the patellofemoral joint (PFJ). TD can be underdiagnosed in up to 73% of cases because the patella tends to spontaneously relocate [3]. Therefore, it is vital to ensure early appropriate diagnosis and to allow management of this condition to be instigated.
The PFJ function is supported by a number of structures that surround the knee joint. Studies regarding the impact and contribution of these structures on patellofemoral stability are sparse in the literature [4]. What prevents the patella from dislocating depends on various static and dynamic structures. The soft tissue provides passive stability, most importantly the medial ligaments (medial patellofemoral ligament) [5,6]. The dynamic stability depends on the anatomical dimensions of the trochlear groove, the normal valgus position of the knee joint (normal limb alignment), and the quadriceps muscles – namely, the vastus medialis [7].
In most cases of TD, the patella dislocates laterally. This is thought to be due to the lateral pulling forces initiated by the lateral quadriceps and patellar tendons [8-10]. The vastus medialis muscle has been found to play an essential role in opposing these forces to provide stability of the PFJ [11,12].
The first-line therapy of managing TD is physical therapy with a combination of proprioceptive exercises, and it is widely accepted that patients should undergo physiotherapy targeting the vastus medialis focusing on muscle strengthening [13-17]. This theory, however, has been questioned because other factors around the knee joint have been found to contribute to the patellar instability [18,19].
The aim of this study was to analyse all the muscle components around the PFJ joint and identify whether gross muscle imbalance could contribute to the stability of the patella in TD.
Material and methods
We performed a retrospective search of our department’s radiology system to identify all patients referred from the knee orthopaedic clinic with suspected trochlear dysplasia over the past 5 years. Within our cohort, all patients underwent cross-sectional imaging computed tomography rotational profiles.
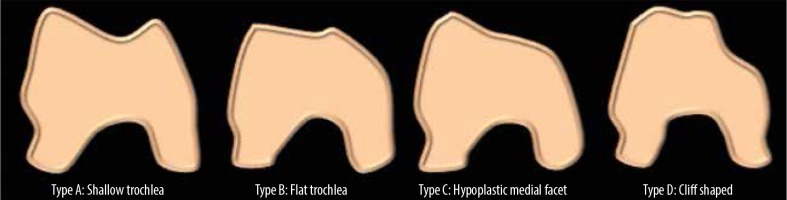
We used Dejour et al. classification to describe the different subtypes of TD obtained in our study [20] (Figure 1).
Type A is characterized by the presence of a shallow trochlea with a prominent ‘crossing sign’.
Type B is distinguished by the presence of a flat trochlear with a supratrochlear spur (on axial CT images) and a ‘crossing sign’.
Type C is characterised by a crossing sign and a double contour sign instead of a trochlear spur.
Type D is typified by the presence of all 3 signs with a sharp convex “cliff” separating the medial and lateral facets on axial CT images.
We calculated the average cross-sectional area ratio (CSAR) of each muscle of the thigh region; the vastus medialis (VM), vastus lateralis (VL), rectus femoris (RF), biceps femoris (BF), semimembranosus and semitendinosus (as one group), the sartorius, and the gracilis. We also evaluated the cross-sectional area (CSA) of each muscle in the specific subtypes of TD and compared this to our normal knee joints within our cohort.
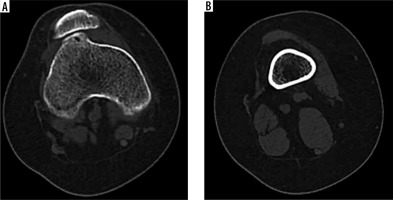
The inclusion criteria included patients with TD or a normal knee joint and no history of previous surgery or existing joint pathologies. Using the ‘cranial’ most slices of CT axial images of the knee joints during extension and in a resting position, we utilized the most proximal measurement (calculated approximately 5 cm proximal to the superior pole of the patella) as a standard to evaluate the CSA of the muscles of the mid-thigh region (Figures 2 and 3).
Figure 2
Diagrammatic animation of the axial of the distal thigh. G – gracilis, ST – semitendinosus, SAR – sartorius

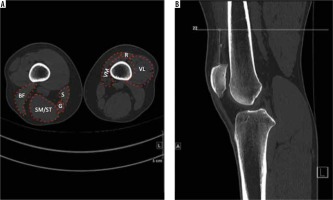
Figure 3
Axial CT (A) and sagittal CT (B) showing the level of measurement of the cross-sectional area of muscles. VM – vastus medialis, VL – vastus lateralis, R – rectus femoris, SM/ST – semimembranosus/semitendinosus, BF – biceps femoris, S – sartorius, G – gracilis
Initially, we compared the CSAR of the quadriceps muscle group against the hamstrings and the medial quadriceps (VM) against the lateral quadriceps (VL), and calculated the p-values using a used a 1-sample t-test to calculate the statistical significance of group differences.
All images were reviewed by 1 consultant musculoskeletal radiologist and 1 senior radiology trainee within our department. It is important to note that there is no known standardized measurement of muscle surface area, and therefore these isolated results are deemed insignificant. We defined the level of significance as p < 0.05 in our study.
Results
We identified 109 consecutive cases in our database, of which 98 patients (196 knees in total) fulfilled the inclusion criteria. Ten cases (20 knees in total) were excluded. The mean age of our patients was 25 years (11-50 years). There was a female-to-male predominance of 67 to 31 (ratio of 2.2 : 1).
Of the 196 knee joints that were reviewed, 10 cases were found to be normal. 186 cases were positive for TD. The majority consisted of the Type C variant, equating to 48.9% (n = 91), followed by Type B TD with 25.2% (n = 47). Type A TD was found in 20.4% (n = 38), and type D TD was identified in only 5.4% (n = 10) of all cases.
We found that the Type B variant of TD had the largest CSA measurement of the vastus medialis (1618.5 mm2) muscle with an overall average of 1451.93 mm2 over all subtypes. Type A TD showed the largest surface area measurement over the vastus lateralis (764 mm2) and rectus femoris muscle (273.3 mm2).
The hamstring muscles showed variable results, with distinctly increased CSA observed over semitendinosus and semimembranosus throughout the TD subtypes (average 1055.60). The rectus femoris was hypertrophied over all TD subtypes except type D (average 208 mm2) (Tables 1 and 2). It was clear that the vastus medialis muscle was larger in comparison to the vastus lateralis muscle over all the different TD subtypes and the normal knee joints, with an average ratio of 2.32 to 1. However, there was no statistical significance between the two muscles, with a calculated p-value of 0.313.
Table 1
The cross-sectional area (mm2) of the muscles of the mid-thigh region over the different subtypes of trochlear dysplasia and normal knee joints in our cohort
Table 2
Table showing the cross-sectional area (mm2) of the muscles of the thigh of all trochlear dysplasia and normal cases in our cohort
There was also a ratio of 1.16 : 1 between the quadriceps and hamstring muscles, and when comparing this to the normal knees within our cohort, the results showed statistical significance (p = 0.014) (Tables 3 and 4; Figures 4 and 5).
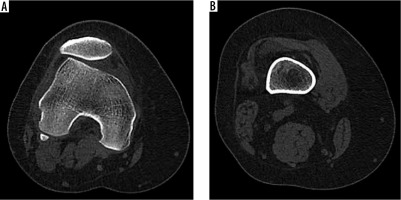
Figure 4
38-year-old male with type B trochlear dysplasia and moderate atrophy of hamstrings and vastus lateralis
Discussion
Trochlear dysplasia is a known condition exemplified by the presence of a shallow and incongruent connection between the patella and trochlear, which leads to recurrent PFJ dislocation [21].
The stability of this joint in a healthy knee depends on different static and dynamic soft tissue structures. Of them, the most important structure is the medial patellofemoral ligament (MPFL), contributing to approximately 60% of the force that opposes lateral displacement of the patella. It acts by providing a restraining force that helps reduce the degree of lateral translation [22]. Along with the MPFL, laterally, the stabilizers are made up of the lateral patellofemoral ligament (LPFL), joint capsule, iliotibial band (ITB), and lateral retinaculum [23-25]. The other important structures include the muscles of the thigh, which have also been shown to provide stability, especially during loading and dynamic movements [26]. The kinematic forces that are supplied by these muscles influence the extent of stabilisation of the PFJ.
Patients with TD suffer from recurrent patellar dislocation; a disabling condition that causes pain, limitation in mobility, and may eventually lead to patellofemoral arthritis. Therefore, diagnoses of TD are essential to ensure early appropriate management is undertaken. Multiple radiographic techniques exist to assess the severity of trochlear dysplasia [27-29]. Both cross-sectional magnetic resonance imaging (MRI) and CT are useful in the diagnosis and evaluation of TD. Moreover, ultrasound imaging is a cost-effective, easily available method that is of particular importance in assessing superficial as well as soft tissue lesions, such as tendinopathies and MPFL tears, which may contribute to patellofemoral instability [30,31].
In various studies, muscle strength (which correlates with force) was found to be directly proportionate to the cross-sectional muscle area (MSCA) [32-35]. When muscle imbalance is present around the patella, patellofemoral diseases may arise. In this study, we concentrated on the distal aspect of the muscles of the thigh, namely the VM and VL and hamstring muscles, with the aim of investigating the size of the different muscles that have been suggested to play a role in the stabilization of the PFJ, and to assess whether muscle imbalance has any significance in guiding the management of TD.
Although the VM muscle is not the most important structure thought to provide stability of the PFJ [4], its importance has been extensively researched and described in the literature [4,11,12,24]. In our study, we found that hypertrophy of the VM and VL muscle was evident throughout the different subtypes of TD, with an average CSA ratio of 2.3 to 1. Whether or not this hypertrophy is due to the natural reaction of the body to counteract the muscular imbalance and prevent the patella displacing laterally is difficult to interpret because this depends on various other static and dynamic structures, as explained previously. Nonetheless, our results correlate with previous studies that have suggested that the restoration of the quadriceps strength and in particular the balance between the VM and VL muscle is considered necessary in offsetting lateral dislocation in TD [36].
Studies regarding the role of the hamstring muscles on the patella and in the stabilization of the PFJ in TD are sparse. The hamstring muscles are composed of the rectus femoris, the semimembranosus and semitendinosus muscles, and possess a biarticular function aiding in hip extension and knee flexion, with medial (by semitendinosus and semimembranosus) and lateral rotation (rectus femoris) of the tibia as the knee is flexed. It is thought that with increased flexion at the knee joint, patients with TD become prone to subluxation and dislocation [37]. This theory stems from the idea that loading of the hamstring muscles causes’ tibial posterior translation and external rotation, increasing the lateral translation of the patella [38-41]. Another concept proposed by Escamilla et al. suggests that activation of the hamstring muscles, along with weakness of the quadriceps and lateral patellofemoral malalignment, can increase the lateral pressures and contribute to lateral patellar dislocation [42]. Based on these theories, it is important to target the quadriceps muscles during rehabilitation exercises, and to attempt to minimize the activation of the hamstring muscles to reduce the risk of dislocation. Overall, although our results show hypertrophy of the hamstring muscles throughout the TD subtypes, and according to the mentioned theories, the increased ratio of quadriceps to hamstring muscles may have assisted in the prevention of patellar dislocation [43].
The role of physiotherapy in trochlear dysplasia
Physiotherapy management is an important intervention for patients who have experienced an episode of instability without evidence of osteochondral injury [44]. Many rehabilitation protocols have been described previously comparing outcomes of non-operative versus operative management in primary acute patella dislocations. These studies have often provided mixed results. Some studies have reported no difference in recurrence rates or subjective functional outcome scores [45-47]. However, other studies have reported significantly lower rates of recurrence and improved outcomes with surgery [48-50]. Physiotherapy for this patient group should take a biopsychosocial approach to the management of this difficult problem and be underpinned by a comprehensive physical examination [51]. The cornerstone of rehabilitation is the restoration of muscular strength and neuromuscular control of the lower quadrant. The programme must ensure optimal neuromuscular rotational control of the joints above and below the knee to prevent dislocation during locomotion [52]. The force-producing capacity of the knee extensors, the hip abductors, and hip extensor musculature is an important target for rehabilitation [53]. This may require a protracted period of intervention to allow adequate recovery of muscle strength for the safe return to physical activities and sport [54]. Additionally, soft tissue flexibility of all structures that could influence patella femoral joint tracking should be assessed and treated to ensure optimal biomechanical balance [55].
Limitations
It is important to note the limitations in this study, and that the results should be interpreted accordingly. One limitation was the fact that we only used axial CT-rotational images, which helped to evaluate the CSA of the thigh muscles but not to assess the total muscle volume. We also did not measure the amount of fatty infiltration, which may add to the CSA but may not correspond with muscle power. Although we calculated the statistical significance between our cohorts, it is essential to note that we did not have a control group to compare this with, because we imaged only symptomatic patients to minimize the risk of CT radiation. But we did have a group of anatomically normal knees according to Dejour classification to offset this. Finally, it is also important to remark that our study measurements were based on static rather than active knee joints, both of which have different biomechanical influences.
Conclusions
The main findings of this study revealed no significant difference in the effect of the thigh muscles CSA on the stability of the PFJ in TD. Further research is required to establish the roles of the different muscles around PFJ in the prevention of TD dislocation, to guide the physiotherapy management. It is important to appreciate the roles of the different static and dynamic structures around the PFJ. Targeting the VM muscle independently does not show any significant improvement in prevention of TD dislocation.