Introduction
Lumbosacral transitional vertebrae (LSTV) denotes the sacralisation of the L5 vertebrae or the lumbarisation of the S1 vertebra. The determination of LSTV is important in many respects. The main task of the sacrum is to correctly convey the body’s weight to the sacroiliac joint [1]. In the presence of LSTV, normal vertebral biomechanics are impaired due to the deterioration of the anatomy. Consequently, instability and early disc degeneration are observed in the presence of LSTV [2]. Disc herniation on the same side and facet joint degeneration are seen more frequently and at a much younger age [3,4]. Pseudoarticulations at the level of LSTV may lead to osteophyte formations and nerve root compressions. The level of the conus medullaris is also affected by the presence of LSTV [5]. In lumbarised S1 vertebrae, the screws should be placed at a wider angle in the sagittal plane [6]. Most surgeries performed at the wrong level have LSTV [7]. People with LSTV may also have dermatome variations [8]. While the vertebrae are enumerated, pilot images containing the cervical, thoracic, and lumbar vertebrae may be obtained and the correct numbering performed, but this may require additional time. For this reason, lumbar magnetic resonance images (MRIs) were evaluated in this study, which aimed to evaluate whether vertebrae can be correctly numbered using auxiliary parameters.
Material and methods
This retrospective study was approved by the Local Ethics Committee. The picture archiving and communication system was scanned for lumbar MRIs performed between October 2011 and January 2016 on patients over 18 years of age. Patients who underwent MRI or computed tomography scans of the whole cervical, thoracic, and lumbar spine were included in the study. Lumbar MRIs were evaluated with consensus by three different radiologists who were blind to the presence of LSTV. Lumbar MRIs were acquired via four different scanners: 1.0 Tesla and 1.5 Tesla (GE Medical Systems, Milwaukee, WI), and 1.5 Tesla and 3 Tesla (Siemens Medical Solutions, Erlangen, Germany). In addition to T1- and T2-weighted images (WI) in the sagittal plane, axial T2-WIs were obtained. The standard imaging protocol is summarised in Table 1.
Table 1
Distribution of paraspinal parameter levels in normal and variational patients (n)
First, only lumbar MRIs were evaluated for the presence of LSTV by assessing the configuration of the vertebrae and the appearance of the lumbosacral angle, regardless of the auxiliary parameters and blind to the whole spine images. Next, the lumbar vertebrae were counted, starting from the C2 vertebrae and counting seven cervical vertebrae and 12 thoracic vertebrae downwards. If there were no differences between the upper and lower end-plateau of the vertebrae, it was evaluated as square or rectangular. If there were five square/rectangular vertebrae up to the sacrum, the patient was assigned to the normal group. If there were four square/rectangular vertebrae, LSTV was identified as sacralisation, and if there were six square/ rectangular vertebrae, LSTV was identified as lumbarisation.
LSTVs were classified using the classification of Castellvi [9]. According to this classification system, type 1 includes unilateral or bilateral dysplastic transverse processes with a length greater than 19 mm, type 2 includes unilateral or bilateral enlarged transverse processes with articulation and adjacent sacral wing, type 3 includes unilateral or bilateral enlarged transverse processes fused with adjacent sacral wings, and type 4 includes type 2 on one side and type 3 on the other. Then, the auxiliary parameters were evaluated: vertebra corpus shape, O’Driscoll classification, lumbosacral axis angle, last two square vertebra dimensions, orifice of right renal artery (RRA), orifice of celiac truncus (CT), orifice of superior mesenteric artery (SMA), vena cava inferior confluence (CVC), abdominal aorta bifurcation (AB), and iliolumbar ligament (ILL).
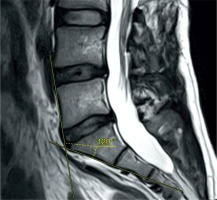
Upper and lower endplates of L5 vertebrae and S1 vertebrae were measured (Figure 1). In patients with small osteophytes, measurements were made starting from the osteophyte border and not included in the osteophytes. When the images were evaluated, patients with a compression fracture (n = 4) or severe osteophyte formation (n = 7) were excluded from the study to avoid misreading the vertebral form. The square/rectangular vertebrae were evaluated as lumbar vertebrae and the trapezoidal vertebrae as sacral vertebrae.
Appeared and true S1 and S2 intervertebral disc morphology was evaluated according to O’Driscoll classification [10]. If there was no disc between the actual S1 and the sacrum, it was identified as type 1, while small residual discs were identified as type 2, and if there was a properly shaped residual disc, it was identified as type 3. If there was an abnormally shaped disc and sagittal sacral axis abnormality due to the squareness of the first sacral element, it was identified as a type 4 disc.
The angle between the upper and lower borders of the last prominent disc was measured (Figure 2). This corresponds to the actual L4-5 disc in sacralised cases and to the actual S1-2 disc in lumbarised cases.
Vertebra dimensions of the middle of the last two lumbar vertebrae corpuses were measured, and the difference was noted (Figure 3).
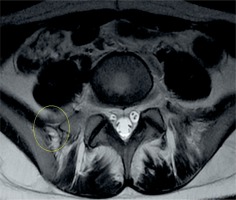
The ILL was determined from the axial slices, and the vertebrae to which it was attached was noted (Figure 4).
Figure 4
The iliolumbar ligament was determined from the axial slices (circle), and the vertebra to which it was attached was noted
The level of the vertebrae corresponding to the level of the origin of the RRA, CT, SMA, CVC, and AB was noted.
Statistical analysis
Statistical analysis was performed using SPSS software. The mean and standard deviation for the age of the patients were calculated. Descriptive statistics were calculated for presacral segments and transitional situations. To verify the reliability of the parameters for determining the transitional segments, we determined the most common level of auxiliary parameters on the basis of the reference standard labelling and expressed this as a percentage. Pearson’s correlation coefficient was performed to find out the relationship of the auxiliary parameters. A p value of < 0.05 was considered significant.
Results
A total of 143 patients (82 females and 61 males) were included in the study. The mean age of the patients was 53.6 ± 16 years (min-max: 18-92). LSTV was observed in 13 (9%) patients. Lumbarisation was detected in six patients (4.1%) and sacralisation in seven patients (4.8%). Seven (54%) of the LSTV cases were female, and six (46%) were male. Lumbarisation was detected in three women and three men, while sacralisation was detected in four women and in three men.
First, lumbar MRIs were evaluated without using any auxiliary parameters. In 11% (n = 16) of cases, segments were wrongly considered. Ten out of 13 patients with variation (76%) were evaluated as normal. Six of the seven patients with sacralisation and four of the six patients with lumbarisation were considered normal. Six of the eight patients who were evaluated as having lumbarisation did not have LSTV (4% of normal cases).
According to Castellvi’s classification, all of the sacralisations were classified into group 3b. Two of the lumbarisations were classified as type 3b, two were classified as 2b, one was classified as 0, and one was classified as type 4.
Vertebra corpus shape
When the vertebra corpus shape was evaluated, the difference between the upper and lower end-plateaus of the L5 vertebrae was 0.13 ± 0.14 mm (0-0.6 mm), and the difference between the upper and lower end-plateaus of the S1 vertebra was 1.29 ± 0.31 mm (0.4-2.2 mm) in the normal group. The difference between the two measurements was statistically significant (p < 0.001). For the correct diagnosis of square vertebrae, the threshold was ≤ 0.65 mm, with sensitivity: 98% (95% CI: 94-99), specificity: 100% (95% CI: 97-100), and accuracy: 99%.
O’Driscoll classification
In the normal group, the S1-2 intervertebral disc was most commonly observed in type 2 morphology as a small residual disc (78%). The appearance of S1-2 intervertebral disc in all cases with lumbarisation was identified as type 2. In the lumbarisation group, the disc between the true S1 and S2 vertebra was seen in type 4 morphology. In the group with sacralisation, the most common type for the visible S1-2 disc was type 3 (57%). The frequency of type 3 discs was significantly higher in patients with sacralisation than in normal cases (p < 0.05).
Right renal artery
In one of the normal cases, the RAA could not be evaluated because the kidney was ectopic. The orifice of the RRA was at the level of the L1 vertebrae corpus in 45% of the normal cases (n = 58/129). In the LSTV group, the orifice of the RRA was at the L1 vertebrae corpus level in 23% of cases (n = 3/13). However, this difference was not statistically significant (p = 0.139). In 75% (n = 97/129) of the cases, the orifice of the RRA was at the level of the L1 vertebra or upper or lower intervertebral discs. In 34% (32/129) of the cases, the orifice of the RRA was at the level of the L2 vertebra corpus.
When there was sacralisation the orifice of the RRA was at the T12-L1 level (n = 4/7, 57%) most commonly, and when there was lumbarisation the orifice of the RRA was most commonly at the level of the L2 vertebrae corpus or more distal segments (n = 4/6, 67%). RRA originated from the level of L1 vertebrae or upper or lower intervertebral discs in 61.5% (n = 8/13) of the variation group and in 75% (n = 97/129) of the normal group, although this difference was statistically insignificant (61.5% vs. 75%, p = 0.225). In 85% (n = 6/7) of the sacralisation group and 33% (n = 2/6) of the lumbarisation group, the orifice of the RRA was at the level of the L1 vertebra or upper or lower intervertebral discs.
Celiac artery
The CA orifice was most frequently observed at the T12 level in the normal group (46%, n = 60/130). In 97.6% of the normal cases (n = 127/130) and 61% of the LSTV group, the CA orifice was located at the area consisting of the T12 corpus, T12-L1 disc, and L1 corpus. This difference was significant p < 0.001. In the group with sacralisation, the most common location of the CA was the area consisting of the T11 corpus, T11-T12 disc, and T12 corpus (n = 6/7, 85%). In cases with lumbarisation, T12, L1, and L2 vertebrae corpuses were observed equally (n = 2, 33.3%).
Superior mesenteric artery
The orifice of the SMA was most frequently at the level of the L1 vertebrae (n = 86/130, 66%) in the normal group. In the LSTV group, the orifice of the SMA was at the L1 level in 80% of cases. This difference was statistically significant (80% vs. 66%, p = 0.015). In the sacralisation group, the most common location was the level of the T12 vertebra (n = 4/7, 57%). In the lumbarisation group, L1 and L1-2 discs were the most common locations (n = 4/6, 66%).
Aortic bifurcation
AB was most frequently observed at the L4 vertebrae level in the normal group (n = 82/130, 63%). AB was significantly more common at the L4 vertebra corpus level in the normal group than in the LSTV group (63% vs. 23%, p = 0.005). The L4-5 disc and L5 vertebra corpus level were found to be most frequent in patients with lumbarisation (n = 3/6, 66%). In cases with sacralisation, AB was most prevalent at the L2-3 and L3 levels (n = 4/7, 57%).
Inferior confluence of the vena cava
CVC could not be evaluated due to compression and variation of the veins in two patients with sacralisation. CVC was frequently observed at the L4 level in the normal group (n = 68/130, 52%). However, CVC was most frequently observed at the L4 vertebra corpus, L4-5 intervertebral disc, and L5 vertebra corpus (n = 120/130, 92%). Comparing the origin of the CVC at the L4 vertebra level in patients with and without variation, a significant difference was observed between the two groups (17% vs. 52%, p = 0.018). In the cases with sacralisation, CVC was most frequently observed in the L3-4 area (n = 3/5, 60%), and in the cases with lumbarisation, CVC was most frequently observed at the L5 level (n = 3/6, 50%).
Angle of the last visible disc
The angle of the last visible disc was 14.2 ± 4 degrees in the normal group and 15 ± 5.4 degrees in the LSTV group. No significant differences were observed between the two groups (p = 0.436). The angle of the visible disc was 13.3 ± 6 degrees in the lumbarisation group and 16.6 ± 4.6 degrees in the sacralisation group, and no significant differences were observed between the three groups (p =0.426).
Vertebra dimensions
The difference between the anteroposterior diameters of the last two square vertebrae was 0.10 ± 0.11 mm (min-max: –0.10 to 0.50 mm) in the normal group, 0.16 ± 0.21 mm (min-max: 0-0.40 mm) in the lumbarisation group, and 0.07 ± 0.12 mm (min-max: 0-0.30 mm) in the sacralisation group. There were no significant differences between the three groups (p = 0.685).
Iliolumbar ligament
Axial sections were scanned for intervertebral discs in routine lumbar MRI examinations. In 6.3% (n = 9/143, seven normal cases and two sacralisation cases) of cases, ILL could not be seen. In all normal cases, ILL originated at the L5 level. In the sacralisation group, ILL was attached to L4 vertebrae in 57% of cases and S1 vertebrae in 14.3% of patients. In the lumbarisation group, ILL was attached to L5 vertebrae in 33% and S1 vertebrae in 67% of the cases.
CA and SMA levels were negatively correlated in normal cases (r = –0.254, p = 0.004). CVC and SMA levels were also negatively correlated (r = –0.248, p = 0.005).
However, there was no correlation between CA and SMA levels (p = 0.441) or between CVC and SMA orifices (p = 0.843) in cases with variation.
Discussion
According to the results of our study, LSTV is quite common (9%). Previous studies have found higher percentages of LSTV (10.6-18.6%) [11-17]. Sacralisation was more common than lumbarisation, which is consistent with other studies (4.8% vs. 4.1%, respectively) [11,14]. Tokgöz et al. found sacralisation and lumbarisation in 10% and 7.6% of patients, respectively [11].
Although it was not statistically significant, LSTV was slightly more common in women in our study (54% vs. 46%). However, in the literature, LSTV is more common in men [17]. Lumbarisation was seen equally in women and men (n = 3). Of the cases with sacralisation, four were female and three were male. In previous studies, lumbarisation was more common in women, and sacralisation was more common in men [6].
In our study, when the lumbar MRIs were evaluated only by looking at the vertebral morphology and lumbosacral axis angle, it was impossible to determine the correct segmentation in 6.2% of the LSTV group. In the literature, this rate was found to be 7% [18]. In fact, in 4.6% of patients with normal segmentation, LSTV was assessed incorrectly. The total error rate was found to be 10.8%. In the study by Tokgöz et al., the error rate was found to be 14% [11]. The correct determination of the vertebral level is critical when planning the intervention. For this reason, auxiliary objective parameters should be used when evaluating routine lumbar MRIs.
Vertebra corpus shape
The first step is to determine the vertebral morphology correctly when determining the transitional vertebra. In previous studies, the ratio between the upper- and lower-end plateaus for differentiating between square- and rhombus-shaped vertebrae was used [11]. In our study, we measured the difference between the end-plates. Accordingly, when the difference between diameters is 0.65 or below, it can be assessed as square vertebra with 99% accuracy.
O’Driscoll classification
Similar to previous studies, the most common morphology of S1-2 intervertebral disc in the normal group was type 2 [17,19]. However, in some studies, the type 3 disc is most common in normal cases [20]. In the same study, the type 3 disc was also the most common type of disc in the LSTV group [20], although this difference was insignificant (43% vs. 36%, p = 0.55) [20]. However, the type 4 disc was significantly more common in the LSTV group than in the normal group (23% vs. 3%, p = 0.004) [20].
In our study, S1-2 intervertebral discs seen in all cases with lumbarisation were observed as type 2. The disc between the true S1 vertebra and the S2 vertebrae was seen in type 4 morphology (a smooth-shaped disc), which has also been reported in the literature [11]. Accordingly, there is a disc similar to the disc between normal L5 and S1 vertebrae between the lumbarised S1 vertebra and S2. Therefore, it seems impossible to differentiate from normal cases by looking at disc morphology in cases with lumbarisation.
In the sacralisation group, the morphology of the visible S1-2 disc was most commonly type 3 (57%) (a properly shaped residual disc). The frequency of type 3 discs was significantly higher in patients with sacralization than in normal cases (p < 0.05). According to the results of Carrino and our study, it could be considered suspicious that the S1-2 disc is in the form of a properly shaped residual disc (i.e. type 3 morphology) [20]. Some studies differentiate the LSTV according to the O’Driscoll classification without separating LSTV into sacralisation and lumbarisation [17]. According to the results of our study, this distinction is critical in the O’Driscoll classification.
Right renal artery
Similar to the literature, the most common origin of the RRA was L1 vertebrae in the normal group (44%). For the normal group, the percentage of the origin of RRA at the L1 vertebrae and lower and upper discs was 81-93% in the literature, whereas it was 75% in our study [11,14,21], and when compared with the LSTV group, there was no statistically significant difference (61% vs. 75%, p = 0.225).
The most common origin of the RRA in the sacralisation group was T12-L1 (57%). In the literature, this rate was lower (29%), and L1 vertebra was the most common site (56%) [11,14]. Similar to the literature, in cases with lumbarisation, the RRA originated at the L2 vertebrae and distal segments (67%) [22].
Celiac artery
The CA originated at the level of the T12 corpus, T12-L1 disc, and L1 corpus in most of the normal cases, which is consistent with the literature [14,21]. In cases with lumbarisation, CA originated at the level of L1 and below (66%), similar to the findings of Jagganathan et al. [14]. In the sacralisation group, CA originated at a higher level [21], but coincided with the normal group at the T12 vertebra level (46%). This finding was also observed in other studies [14]. The CA’s origin was one of the parameters with a significant difference between the groups with and without variation, but the area under the curve was quite low (p < 0.001, AUC: 0.681).
Superior mesenteric artery
Tokgöz et al. found that SMA is much more frequent at the L1 level, similar to this study (66% vs. 14% and 55% and 31%) [11]. Lee et al. also showed that the L1 level was the most common (67.9%) [21]. The orifice of the SMA was most frequently at the level of the L1 vertebrae (n = 86/130, 66%) in the normal group. Jagganathan et al. found that the SMA origin was most frequently at the T12-L1 level in the normal group (46.9%), followed by the L1 level (31.9%) [14]. However, when T12-L1 and L1 levels were combined, the percentages were similar (79% vs. 77%) [14].
In the LSTV group, the orifice of the SMA was at the L1 level in 30% of cases. This difference between the LSTV and normal group was statistically significant (30% vs. 66%, p = 0.015). In the group with sacralisation, it was found to be one level up, and the most common level was the T12 vertebra (n = 4/7, 57%). Similarly, in the literature, the T12 vertebra (42%) was the most common location [11,14], and these rates were increased when T12 and T12-L1 levels were considered, to 71% in our study and to 87% in the literature [22]. In cases with lumbarisation, L1 and L1-2 discs (66%) were the most common level, which is consistent with the literature (66-86%) [11,14,22]. The origin of SMA at the level of the T12-L1 intervertebral disc and L1 vertebrae corpus was significantly more common in the normal group than in the variation group (80% vs. 38%, p = 0.002). When T12-L1 and L1 levels were evaluated, the area under the curve was higher than the other auxiliary parameters (AUC: 0.712).
Aortic bifurcation
AB was most commonly seen at the L4 vertebrae level (63%). This rate was found to be 45% in the study by Jegganathan et al., while higher frequencies have been reported in the literature (70%, 83%) [14,21,22]. Similar to the literature, L4-5 disc and L5 vertebra levels were more frequent in patients with lumbarisation (66%), and this rate was found to be higher in other studies (88%) [22]. L2-3 and L3 levels (57%) were the most common location of orifices in patients with sacralisation, but Lee et al. and Jegganathan et al. found L3-4 and L4 levels with frequencies of 91% and 73.9%, respectively [14,22].
Confluence of the inferior vena cava
CVC was most commonly observed at the L4 level (52%), similar to the literature (47%) [14], and when L4 and L5 vertebrae corpuses and L4-5 intervertebral disc region were considered, the frequency increased to rates similar to those reported in the literature (92%) [14]. Frequencies reaching 95% were also reported [22]. The most common level was L3-4 (n = 3/5, 60%) in cases with sacralisation and L5 in cases with lumbarisation (n = 3/6, 50%). According to a study conducted by Jagganathan et al., in the sacralisation group, the L4 vertebra level was more common than the L3-4 level (47.8% vs. 32.6%) [14]. When the orifice of the CVC at the level of the L4 vertebrae in the normal and LSTV groups was compared, there was a significant difference between the two groups (17% vs. 52%, p = 0.018). It has already been reported that the angle of the lumbosacral junction is not diagnostic [20]. This was also confirmed in our study, indicating that there are no significant differences between the normal and LSTV groups (p = 0.436), and there were no statistically significant differences in the sacralisation group compared to the normal group and the lumbarisation group (p = 0.426).
Vertebra dimensions
The dimensions of the last two square/rectangular vertebrae were measured in this study. This measurement was made based on the idea that the difference between the size of the two vertebral bodies in lumbarised or sacralised patients varies (i.e. the transitional vertebrae may be smaller or larger). However, the difference between the dimensions of the last two square vertebrae was not statistically significant (p = 0.685). As far as we know, this diameter difference has not been reported previously in the literature.
Lumbosacral axis angle
It has already been reported that the angle of the lumbosacral junction is not diagnostic [20]. This was also confirmed in our study, indicating that there is no significant difference between the normal and LSTV groups (p = 0.436). Also, there was no statistically significant difference in the sacralisation group compared to the normal group and the lumbarisation group (p = 0.426).
Iliolumbar ligament
In the anatomy literature, it is reported that ILL attaches the L5 vertebrae transverse process [23]. There are studies suggesting that ILL extends from L5 vertebrae in all normal cases [20]. It was observed that ILL may extend from other vertebrae than L5 in patients with LSTV [17,20,22]. In the literature, the origin of ILL from the L5 vertebra is significantly higher in normal cases than in patients with LSTV [16,17,20,24]. In our study, although ILL attached the L5 vertebra in all of the normal cases that could be detected, we were unable to observe ILL in 6.3% of the cases. Hughes et al. were unable to detect ILL in 9% (n = 46/500) of cases, and Carrino et al. were unable to detect ILL in 14% of cases (n = 21/147) [16,20]. In the literature, it has been reported that ILL may be smaller due to the excessive development of the transverse process in some cases [25]. Also, ILL may not be detected because the ILL does not enter the cross-section in axial sections, which are focused in the intervertebral discs. It may be necessary to take continuous sections to display the ILL [16], but this may not be cost-effective. Additionally, it has been reported that there may be weak connections with the L4 vertebrae and it can be observed as two bands of L4/L5 and L5/S1 [14,16,22].
Limitations
This study has some limitations. First, although there was no bias in the selection of the patients, the patients included in the study were a group who received a complete spinal examination rather than patients who were examined within a specific date range. The patients included in the study had low back pain, so the asymptomatic population was not included in the study. Additionally, the study was retrospective, and the small number of patients with variation reduces the reliability of the study.
Conclusions
According to the results of our study, no single parameter in the MRI can accurately indicate the number of vertebrae without counting the levels. Although the vascular structures are helpful, their position may change with age [26]. As a result, we believe that these parameters may be suspicious in terms of the presence of LSTV rather than the correct level. Although lumbarisation and sacralisation are categorised as LSTV, they are actually completely different.