Introduction
There has been a massive outbreak of a novel coronavirus infection since December 2019 [1]. The virus, presently known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or coronavirus disease 19 (COVID-19) or new coronavirus 2019 (2019-nCoV), manifests with respiratory disease of variable severity. It attained pandemic proportions according to the World Health Organisation on March 11, 2020 [1].
The typical symptoms of COVID-19 infection are fever, dry cough, fatigue, sputum production, shortness of breath, myalgia or arthralgia, sore throat, headache, chills, nausea or vomiting, nasal congestion, diarrhoea, haemoptysis, and conjunctival congestion [1]. COVID-19 infection is confirmed using the reverse transcriptase polymerase chain reaction (RT-PCR) test [1].
Currently, imaging is not recommended for screening or diagnosis of COVID-19 infection [2-4]. Imaging should not be used to determine the need to test a patient for COVID-19. A normal chest radiograph or chest computed tomography (CT) does not exclude COVID-19 infection, while an abnormal study is not pathognomonic for COVID-19 diagnosis [2-4]. Imaging should be used to only answer definite clinical questions in symptomatic in-patients (e.g. suspected pulmonary embolism, distinguishing organising pneumonia from acute respiratory distress syndrome [ARDS], excluding stroke or encephalopathy in those with neurological symptoms, etc.) [2-4].
Radiologists and other physicians need to be well acquainted with the radiological features of COVID-19 infection because the disease may be encountered in patients imaged for other indications. The purpose of this review is to illustrate the imaging manifestations of COVID-19 pictorially.
Chest radiography
Chest radiography is readily available and affordable. Though it has limited sensitivity for COVID-19 infection, it is still a first-line modality that can also be used for follow-up and evaluation of complications [2]. The common findings on chest radiography (consolidation, ground-glass opacities) are usually bilateral and peripheral, with lower zone predominance [5]. There have also been reports of spontaneous pneumomediastinum. Unfortunately, chest radiographs may be normal in the early stages or mild forms of the disease. Figures 1-6 illustrate the plain chest radiographic features of RT-PCR-confirmed COVID-19 infection.
Figure 1
Posteroanterior chest radiograph of a 56-year-old COVID-19- positive man, showing streaky opacities in the left lower lung zone (arrows)

Figure 2
Posteroanterior chest radiograph of a 45-year-old COVID-19-positive man, showing bilateral ground-glass opacities more peripherally and predominantly in the mid and lower lung zones. An endotracheal tube is in-situ

Figure 3
Anteroposterior chest radiograph of a 65-year-old COVID-19- positive man, showing extensive ground glass opacities and multifocal areas of consolidations (arrows) in bilateral (right > left) middle and lower zones

Figure 4
Chest radiograph (AP view) of a 49-year-old COVID-19-positive man. There are diffuse bilateral consolidations (more on the right) with scattered areas of ground glass opacities (more in the left lung). There is associated air bronchogram within the opacities. Relative sparring of both lung apices is noted. No pleural effusion
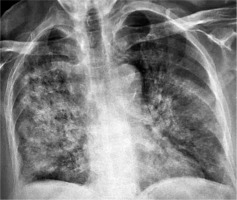
Figure 5
Chest radiograph (AP view) in a 59-year-old COVID-19-positive man, showing extensive bilateral pulmonary consolidation with air bronchograms
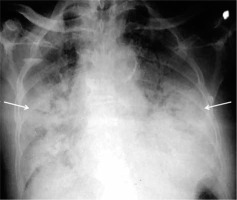
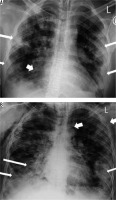
Figure 6
The above pair of CXR (AP view) is for a 38-year-old man with COVID-19 infection, who was examined twice, four days apart. On day 1 (A), there are predominantly peripheral opacities bilaterally (thin arrows) and right paracardiac consolidation with an air-bronchogram (thick arrow). Follow-up radiograph on day 5 (B) shows a progression of the ground-glass opacities and consolidations (thin arrows) with development of spontaneous pneumomediastinum and subcutaneous emphysema (thick arrows)
Chest computerised tomography
Non-contrast (plain) chest CT at 0.625-1.5 mm slice thickness is the standard protocol for COVID-19 patients. A pre-contrast study is necessary for those who require contrast administration (e.g. suspected pulmonary embolism, history of haemoptysis); otherwise, accurate interpretation of ground-glass opacities might be diffi-cult [6].
The notable findings on chest CT are depicted below.
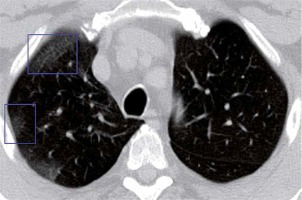
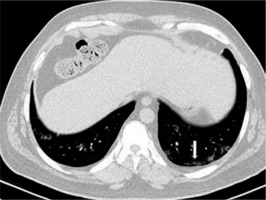
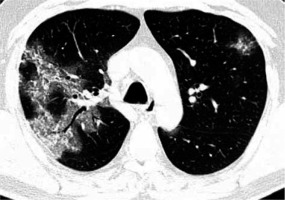
Ground-glass opacities
Ground glass opacities (GGO) are foggy opacities that do not conceal the underlying bronchial structures or pulmonary vessels (Figures 7 and 8). GGO maybe as a result of partial exudate or transudate filling the air spaces of the lungs, as well as an interstitial thickening or partial collapse of the alveoli [7]. In COVID-19 patients, GGO is usually bilateral, multilobar, peripherally or posteriorly distributed (or both), and usually in the lower lobes.
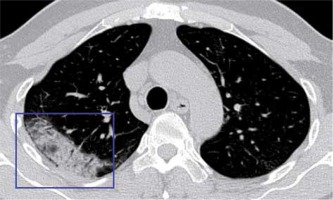
Consolidation
Consolidation occurs when pathological fluids, tissues, or cells replace alveolar air, causing opacification due to the increase of pulmonary parenchymal density obscuring the underlying vessels (Figure 9) [7,8] Consolidation often becomes the second most predominant finding about 14 days after the onset of the disease [7]. It could be patchy or multifocal, and its presence may indicate increased severity [8].
Air bronchogram
Air space consolidations are air- or gas-filled bronchi surrounded by grey or white alveoli made visible on a background of opaque (high attenuation) airless lung (Figure 9) [7,8]. Air bronchogram characterises air space consoli-dation.
Nodules
Nodules are rounded irregular, poorly defined opacities that measure about 3 cm diameter [8]. They can be micronodular or macronodular. They can also be classified into discrete focal nodules and centrilobular or ‘tree in bud nodules’. Nodules have been reported in 3-13% of COVID-19 patients, appearing as multifocal solid irregular nodules (Figure 10), sometimes with a visible halo sign [4,9]. However, centrilobular nodules are infrequent in COVID-19.
Pleura affectation
Pleural thickening (common; seen in about 56%) and pleural effusion (uncommon) may be present in COVID-19 [3,9]. The presence of pleural effusion should alert to the possibility of underlying immunocompromised sta-tus [10].
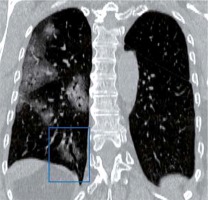
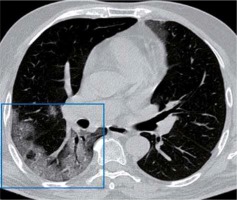
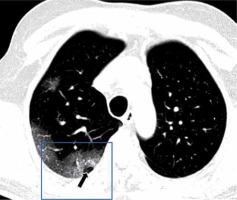
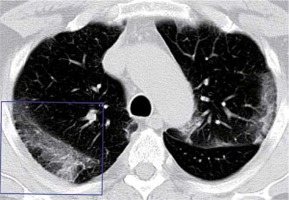
Subpleural lines
The subpleural line is a thin curvilinear opacity of about 1-3 mm in thickness found close to the pleural surface (Figures 11 and 12) [11]. It is located in the subpleural region and is distributed parallel to the pleural surface. It is a non-specific sign, seen in 33.9% of COVID-19 cases, but can also be caused by dependent atelectasis, pulmonary oedema, and fibrosis [11]. Subpleural lines may be related to the predominantly peripheral location of parenchymal changes in COVID-19.
Fibrosis
Fibrotic lesions may occur due to the replacement of cellular components by scar tissues in patients with proliferative diseases and patients recovering from chronic pulmonary inflammation (Figure 13) [9]. Fibrosis in COVID-19 is usually not seen at the early stage until 2-3 weeks when interstitial changes begin to occur [4] Some studies argued that the presence of fibrosis indicates advanced COVID-19 [12], which could lead to bronchus deformation. In contrast, others opined that it depicts healing [9].
Halo sign and atoll sign
The halo sign comprises masses that surround GGO [12]. It is related to perilesional haemorrhage in angioinvasive fungal infections, hypervascular metastases, viral infections, and organising pneumonia [12]. However, the pathogenesis of halo sign in COVID-19 is unknown [12]. Halo sign, together with other characteristic manifestations (vascular thickening, air bronchogram sign, and crazy-paving pattern), is usually associated with GGO at the early onset of COVID-19 [12]. Reversed halo sign may indicate a developed stage of COVID-19, and it is associated with the consolidation of GGO [12]. On CT, a “reversed halo sign (atoll sign)” (Figure 14) and/or pulmonary nodules with a halo sign may be seen in COVID-19 [9].
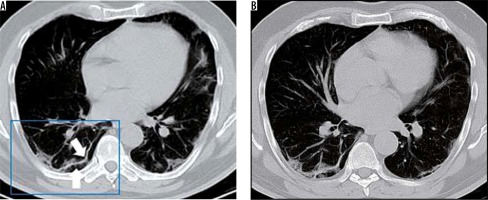
Cavitation and air bubble sign
Cavitation is notably uncommon in COVID-19 patients [7]. However, air bubble sign or bubble-like air-containing space, which is a small air-containing space associated with bronchiolectasis (Figure 15), has been termed “cavities” by some authors [12].
Airway
Bronchiectasis and bronchial wall thickening are features of COVID-19 infection (Figure 16) [12]. Bronchial wall thickening is predominant in more critical COVID-19 cases compared to mild cases [12]. They are caused by bronchial obstruction and inflammatory damage of the bronchial wall, which leads to tractive bronchiectasis, fibrosis, fibrous tissue proliferation, and destruction of the bronchial wall structure [12].
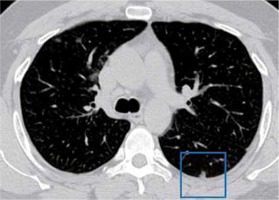
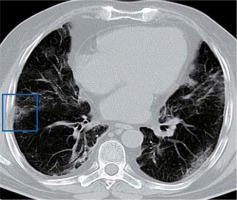
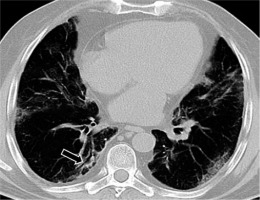
Crazy-paving appearance
The crazy-paving pattern is produced by ground-glass opacity overlaid on a web of linear opacities. The linear opacification may be due to superimposed thickened intralobular lines and interlobular septa (Figures 17 and 18) [9]. It is rare in COVID-19, where it could characterise a developed stage at about the third week after the onset of symptoms [9].
Bronchiectasis
Bronchiectasis and bronchial wall thickening are airway changes, which may be due to obstruction of the bronchi (damaging the structure of the wall), inflammation of the bronchial wall, proliferation of fibrous tissue, tractive bronchiectasis, and fibrosis. Bronchiectasis is seen in 10-20% of COVID-19 patients [8].
Vascular changes
Vascular dilatation or widening of the pulmonary vessels is a typical feature within GGO [12]. It may be caused by pro-inflammatory factors, which result in damage and oedema of the capillary wall [12]. It is observed as early as the first week of onset but does not exhibit the irregular dilatation and convergence seen in malignant lesions [12].
Lymphadenopathy
Lymphadenopathy may manifest as early as the first week in some COVID-19 patients, and towards the third week in others [9]. Its occurrence alongside tiny nodules and pleural effusion may signify a bacterial superinfection. Lymphadenopathy has been reported in 4-8% of patients. It is a marker of severity [9].
Imaging differential diagnoses of COVID-19 infection
The common differentials include viral pneumoniae, atypical pneumonia (Chlamydophila pneumoniae, Mycoplasma pneumoniae, Legionella pneumophilia), acute eosinophilic pneumonia, acute interstitial pneumonia, cryptogenic organising pneumonia, acute pulmonary oedema (cardiogenic and non-cardiogenic), and interstitial lung disease [6].
Ground-glass opacity (91% vs. 68%), peripheral distribution (80% vs. 57%), vascular thickening (59% vs. 22%), and fine reticular opacity (56% vs. 22%) are more predominant in COVID-19 pneumonia than in non-COVID-19 pneumoniae, whereas pleural effusion (4.1% vs. 39%), lymphadenopathy (2.7% vs. 10.2%), and concurrent central and peripheral distribution of lesions (14% vs. 35%) are less common in COVID-19 pneumonia than in non-COVID-19 pneumoniae [13].
Chest ultrasonography
The stage of the disease, extent of lung damage, and the presence of comorbidities determine the sonographic features of COVID-19 pneumonia. The posterobasal aspects of the lung fields are the most common sites of COVID-19 affectation on ultrasonography [6,14].
The sonographic features of COVID-19 pneumonia include irregularly thickened and discontinuous pleural line, the appearance of B lines (focal, multifocal, or confluent), subpleural consolidations, alveolar consolidation with static or mobile sonographic air bronchograms/air bronchiolograms, and return of bilateral A lines during recuperation (restoration of aeration during recovery) [6,14].
Neuroimaging in COVID-19
A neurological complication of COVID-19 infection that may require brain imaging is acute haemorrhagic necrotising encephalopathy (AHNE) [15]. AHNE lesions are hypodense on CT and hyperintense on T2 FLAIR MRI with internal haemorrhage. Ring enhancement may be seen after intravenous contrast [15]. The lesions are characteristically symmetric, multifocal, and always involve the thalamus. The supratentorial white matter, cerebellum, and brain stem may also be affected [15]. Cerebrovascular accident (stroke) has also been reported in patients with COVID-19 infection [16].
PET-CT hybrid imaging
The pulmonary ground-glass opacities in COVID-19 show increased avidity for 18-fluorodeoxyglucose (FDG). Furthermore, patients whose pulmonary lesions exhibit higher standardised uptake value (SUV) may take longer to recover [6].