Introduction
Temporomandibular disorder (TMD) is an umbrella term that encompasses several clinical entities that affect the temporomandibular joint (TMJ) or extraarticular structures, as described by the expanded taxonomy for TMDs, which was developed by the American Academy of Orofacial Pain (AAOP) in 2014 [1]. It is the second most common chronic musculoskeletal condition after chronic low back pain. While imaging may not be required for the diagnosis of extraarticular disorders, it is typically needed for a definitive diagnosis of TMJ intra-articular disorders according to the Diagnostic Criteria for TMD (DC-TMD) scheme [2]. Among the TMJ intra-articular disorders, internal derangement of the disc and joint mechanics is the most frequent type of disorder [3].
Internal derangement (ID) of the TMJ is defined as an abnormal positional and functional relationship between the disc and articulating surfaces. Common clinical symptoms include pain and joint sounds (clicking or crepitus) [4]. It is important for the radiologist to detect early imaging signs of internal derangement, thereby avoiding the evolution of this condition to degenerative joint disease [5].
Magnetic resonance imaging (MRI) is the reference standard for evaluating the articular disk and softtissue structures of the TMJ. Computed tomography (CT) is most useful for evaluating osseous changes [3]. This pictorial review demonstrates the imaging findings in internally deranged TM joints on 3T MR and multiple detector computed tomography (MDCT). The aim of this article is to familiarise the reader with the spectrum of imaging findings that are encountered at different stages of the disease. A brief discussion on TMJ hypermobility has also been included because it is associated with ID.
Normal anatomy
Temporomandibular joint is a ginglymoarthrodial joint between the mandible and the squamous part of the temporal bone. It is a complex synovial articulation with hinge, sliding, and rotational motions. The osseous components are composed of the mandibular condyle inferiorly and the glenoid fossa and articular eminence superiorly. The joint is divided into a superior joint space and a smaller inferior joint space by a biconcave, fibrous structure, called the TMJ disc. The TMJ disc has three distinct segments: an anterior band, an intermediate zone, and a posterior band. Both the anterior and posterior bands are triangular in shape and are connected by a thin intermediate zone (Figure 1A). The disc has a low signal intensity appearance on all MR sequences.
Figure 1
Normal anatomy. A) Sagittal oblique view (closed mouth). B) Sagittal oblique view (open mouth). C) Coronal oblique view (closed mouth)

In the coronal plane, the disc has an arc-shaped configuration, with the medial margin of the disc attaching to the neck of the condyle just inferior to the medial pole. The lateral margin is attached just underneath the lateral pole of condyle. The posterior band of the disc should be centred on top of the condyle on both closed and open mouth views (Figure 1C). The disc merges around its periphery into the surrounding capsule.
Dynamic stability is provided to the disc by several ligamentous attachments. The main stabilising force for the TMJ is the posterior attachment (PA) or bilaminar zone. The PA has been divided into three parts: the temporal PA (TPA) (a.k.a. the superior lamina), the intermediate part of the PA (IPA), and the condylar PA (CPA) (a.k.a. the inferior lamina).
On a typical MR examination (Figure 2), a normal disc position is defined according to the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) as follows:
Figure 2
Normal anatomy of the temporomandibular joint (closed mouth). Sagittal oblique proton density fat saturation (A) and coronal oblique T1W (B) images show thin cortical outline (white arrow), disc in normal position with junction of posterior band (PB) and posterior attachment (PA) at 12 o’clock position (yellow arrowhead), smooth cortical outline of glenoid fossa and articular eminence (white arrowhead) with normal joint space. Axial T1w (C) and STIR (D) images show oval shaped condylar head (yellow arrow) with normal bone marrow signal (asterisk)
junction of posterior band (PB) and PA located between 11:30 and 12:30 clock positions on sagittal oblique view (with maximum intercuspation), and
intermediate zone (IZ) located between the anterior-superior aspect of the condyle and the posterior-inferior aspect of the eminence.
Normal TMJ function requires synchronised and coordinated motion of the disk, condylar head, and the muscles of mastication. In the maximum open mouth position, the condylar head should be positioned inferior to the articular eminence and the disk assumes a bow-tie configuration, with the thin intermediate zone situated between the articulating surfaces of the mandibular condyle and the articular eminence (Figures 1B and 3) [6].
Figure 3
Normal anatomy of temporomandibular joint (open mouth). Sagittal oblique T2W-FS (A) and proton density fat saturation (PD-FS) (B) images show normal anterior translation of condylar head (asterisk) below the articular eminence (white arrow) with disc interposing between them (white arrowhead). Retrodiscal tissue (yellow arrow) appears normal and is better assessed on T2W images. Coronal oblique PD-FS (C) shows normal disc signal and position (yellow arrowhead). The signal of the disc is better assessed on PD images
Technique
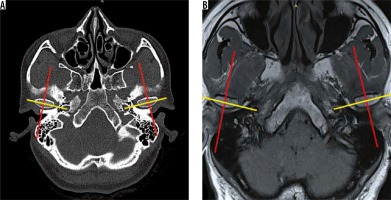
Computed tomography technique
With patient in a supine position, non-contrast high-resolution CT scan of bilateral TMJs is performed. Coronal oblique images are reconstructed along the horizontal long axis of the head of the mandibular condyle. Sagittal oblique images are obtained perpendicular to this plane (Figure 4). TMJ is evaluated for the morphology of condyle, glenoid fossa, articular eminence, and joint space.
Magnetic resonance imaging technique
Multiplanar magnetic resonance imaging of bilateral TMJs is conducted using a phased array or surface coil. A typical MR study includes the following sequences: T1 W (T1 weighted) axial and coronal oblique closed mouth, T2 W FS (T2 weighted fat suppressed) sagittal oblique closed and open mouth, PD FS (proton density fat suppressed) sagittal oblique closed and open mouth, PD FS (proton density fat suppressed) coronal oblique open mouth, STIR axial/coronal closed mouth, and T2 W Cine (dynamic MR). The disc and surrounding soft tissues are best evaluated on MR.
Internal derangement
Internal derangement is defined as an abnormal relationship of the TMJ disk to the mandibular condyle, articular eminence, and glenoid fossa and may affect up to 28% of the population. The exact aetiology of internal derangement remains a subject of debate, although a history of recent trauma can sometimes be elicited [7].
Epidemiology
The symptoms appear in the second to fourth decades with a peak incidence seen at puberty [7]. Higher female prevalence has been described in the literature, with a female-to-male ratio of up to 2.5 : 1 [8,9]. The factors responsible for higher incidence in females are not known; however, it has been suggested in animal studies that joint laxity involving any joint occurs more commonly in females, and individuals with joint laxity as a result of altered collagen synthesis are at greater risk of developing bilateral TMJ dysfunction when subjected to aetiological factors such as trauma, joint overextension, or joint over-use. Another biochemical hypothesis suggests the role of oestrogen and relaxin in the induction of matrix metalloproteinase and cytokines that cause tissue breakdown [6].
Contralateral asymptomatic joints of patients with internal derangement also commonly show disc displacement. Bilateral affection of the TMJs has been observed in 60-63% of examined patients with internal derangement [9-11]. The reason for the high incidence of bilateral involvement of the TMJs is unknown. However, it has been hypothesised that patients who have a prior history of injury or trauma to the head, neck, or jaws may have sustained either direct or indirect damage to both the TM joints. Any exogenous factor that may participate in the development of internal derangement in one TMJ may lead to development of internal derangement in the contra-lateral joint as well. While sometimes symptoms may be present in both joints, the patient may experience pain and dysfunction of greater intensity and severity on one side [10].
Clinical features
The clinical signs and symptoms of internal derangement within the TMJ are described collectively as TMJ syndrome. It is considered to be a progressive disorder. Symptoms of internal derangement typically include craniofacial pain, joint-clicking or popping, and reduced mouth opening.
Joint pain in internal derangement has been attributed to various mechanisms including squeezing of the PA between the condyle and articular eminence, trauma from the disc impinging on the inner aspect of the anterior capsule, and secondary inflammatory changes (capsulitis and discitis) [6]. Pain is characteristically seen in acute disc displacement without reduction.
Early stages of disc displacement are characterised by clicking. Clicking can be heard while opening the mouth, while closing the mouth, or both. An opening click signifies recapture of the displaced disc between the articulating joint surfaces. A closing click occurs just prior to tooth contact and is not as loud as the opening click. When the disc becomes non-reducible, i.e. there is no recapture of the disc while opening the mouth, the clicking reduces in intensity or vanishes.
In the early stages (disc displacement with reduction), patients have been described as having increased range of anterior condylar translation. As the stage of disc displacement without reduction ensues, the patient encounters reduced mouth opening and even locked closed in some cases.
Several studies have reported a significant association between TMJ pain and joint effusion as well as between TMJ pain and bone marrow oedema of the mandibular condyle [12]. Histologic findings of core biopsy specimens from the bone marrow of the mandibular condyle have been shown to correlate well with preoperative MRI observations in patients undergoing surgery for painful IDs. An in-patient regression analysis of the side differences in TMJ pain, in which the patient was his/her own control, demonstrated that the pain was significantly dependent on fluid as well as bone marrow abnormalities [11]. Significant associations have also been studied between TMJ pain and the MRI findings of disc displacement without reduction and severe degenerative joint disease [12].
Pathophysiology and imaging findings
In internal derangement, there is an abnormal anatomic relationship of the fibrous disk with the condylar head. Initially, soft tissue changes occur, following which osseous changes are seen. As the disease progresses, a variety of soft tissue changes can be encountered in the joint, which are picked up on MRI. Disc displacement, disc signal morphological alterations, and PA remodelling are seen as early changes in the pathophysiology of the internal derangement and degenerative joint disease (ID-DJD) spectrum. These are later followed by osseous changes and development of degenerative joint disease. This sequential progression from internal derangement to degenerative joint disease has been described by Tamimi et al. [6] based on correlation of clinical and radiological findings (Table 1).
Table 1
Sequential progression of internal derangement injury and degenerative joint disease
I. Abnormal disc position/morphology/signal
A. Position: Disc displacement can occur in any anatomic direction. However, the four general categories are:
Anterior displacement (ADD): disc anteriorly displaced on oblique sagittal sections, without lateral and medial displacement on coronal oblique images (Figure 5).
Sideways displacement:
Anterior rotational displacement:
anterolateral (ALDD) – disc anteriorly displaced on oblique sagittal sections, with lateral displacement on coronal sections (Figure 6);
anteromedial (AMDD) – disc anteriorly displaced on oblique sagittal sections, with medial displacement on coronal sections.
Posterior disc displacement (PDD) – disc posteriorly displaced on oblique sagittal sections (Figure 7).
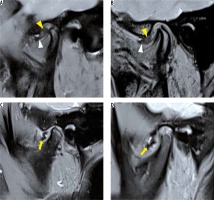
Figure 5
A-C) Anterior disc displacement. Sagittal oblique proton density fat saturation (PD-FS) magnetic resonance image (A) reveals junction of posterior band (PB) and posterior attachment (PA) at 8 o’clock position (yellow arrowhead) of the condyle. Coronal oblique T1W (B) and PD-FS (C) images reveal non-visualisation of disc superior to the condyle (yellow arrow) with joint space reduction with visualisation of the disc on an anterior section (white arrowhead)
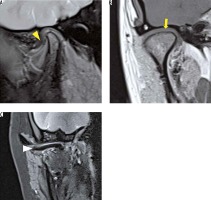
Figure 6
Antero-lateral disc displacement. Sagittal oblique proton density fat saturation magnetic resonance images (A, B) reveal junction of posterior band (PB) and posterior attachment (PA) at 11 o’clock position in the central section with visualisation of the disc on a far lateral section (white arrow). Coronal oblique T1W images (C, D) show non-visualisation of disc superior to the condyle (yellow arrow). A more anterior section (D) shows hypointense disc (white arrow) on lateral aspect
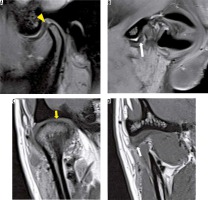
Figure 7
A, B) Posterior disc displacement. Sagittal oblique proton density fat saturation closed (A) and open mouth (B) show the junction of PB and PA at 2 o’clock position with perforation of disc at the intermediate zone (IZ) (white arrowhead)
Anterior and anterolateral disc displacement have been found to be the most common types [11]. Sideways disk displacement is less commonly seen [13]. One possible explanation for the rarity of sideways disc displacement compared to anterior disc displacement is that the anterior direction is the line of least resistance for disc movements, whereas the medial and lateral surfaces are more firmly supported by their ligaments [9].
In an open mouth position, a displaced disc is again analysed in both sagittal and coronal planes to classify as complete reduction (wR), partial reduction (wpR), or without reduction (woR).
Disc displacement with reduction (DDwR) indicates that the displaced disc position in the closed jaw position returns to a normal superior position relative to the condyle during jaw opening (Figure 8). This condition is frequently associated with clicking. During closing of the jaw, the disc is again anteriorly displaced, and this is also associated with a softer click. This type of dual clicking has been termed reciprocal clicking.
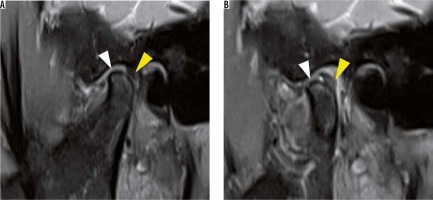
Figure 8
A-C) Disc displacement with reduction (DDwR). Sagittal oblique Proton density fat saturation (A) and coronal oblique T1W (B) images reveal junction of posterior band (PB) and posterior attachment (PA) at 11 o’clock (yellow arrowhead in A) with non-visualisation of disc superior to condyle (yellow arrow in B), suggesting anterior disc displacement. Open-mouth sagittal oblique T2W-FS (C) image shows reduction of disc in open-mouth position (yellow arrow)
Disc displacement with partial reduction (DDwpR) indicates a disc that is displaced in both coronal and sagittal oblique planes in closed mouth position and reduces only in the sagittal oblique plane in the open mouth position.
Disc displacement without reduction (DDwoR) is a terminology indicating that the disc remains in a displaced position during all mandibular movements (Figure 9).
Figure 9
A, B) Disc displacement without reduction (DDwoR). Closed-mouth (A) and open-mouth (B) sagittal oblique proton density fat saturation images show anterior disc displacement (white arrow), which is seen to displace further anteriorly (yellow arrowhead) on open-mouth position
Disc displacements with complete or partial reduction are more commonly observed than DDwoR.
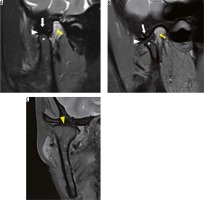
B. Morphology: A normal disc has a biconcave shape. Altered morphologies of discs, like posterior band (PB) thickening, shortening of AP dimension, bending/crumpling or perforation, are recorded (Figure 10). Crumpled disc is seen more commonly in joints with DDwoR than in those with DDwR [9].
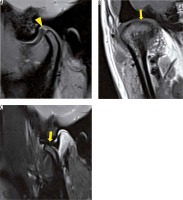
Figure 10
A-D) Patterns of altered disc morphology. In 4 different patients with internal derangement, sagittal oblique proton density fat saturation magnetic resonance images show thickening of posterior band (PB) (yellow arrowheads) (A, B); shortening of antero-posterior dimension of disc with small intermediate zone (IZ) (white arrowheads) (A, B); and crumpled disc (yellow arrows) (C, D). Also note the abnormal intermediate signal of disc (A, B)
C. Signal: A normal disc should have low signal intensity on all sequences. The presence of a high signal is considered abnormal (Figure 10).
II. Fine structural changes with disc displacement
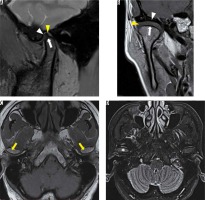
PA remodelling – Fibrosis of the anterior part of the PA develops, and the configuration of the posterior disc attachment sometimes also changes to resemble the posterior band of the disc. This gives a pseudo-disc appearance (Figure 11). PA remodelling and fibrosis is evident by T2 hypointense signal within PA as well as thickened superior and inferior laminae of PA.
Perforations – When the remodelling process is not adequate for the degree of anatomic and functional abnormalities, the tissues become irreversibly damaged, and perforations of the posterior disc attachment may occur. These cannot be clearly demonstrated by MR unless there is sufficient joint fluid. When joint fluid is present, T2-weighted MR imaging can aid in depicting the perforation of the disc owing to the “arthrogram effect” image obtained. However, studies have shown that MR has a low sensitivity in detecting perforations of disc and PA when compared with arthrography, which is considered as the gold standard.6 Perforations associated with disc displacements are more commonly seen in the posterior attachment rather than in the disc itself, and in late stages they are associated with arthrosis.
Lateral pterygoid muscle (LPM) tendon thickening – Additional soft tissue abnormalities with chronically displaced discs include actual thickening of the tendinous insertion of the inferior belly of the LPM to the condyle, and thickening of the fascial coating of the inferior belly of the LPM, which may also give a pseudo-disc appearance.
Type of LPM attachment – LPM attachment can further be classified on PD FS closed-mouth sequence into types I, II, and III, based on its insertion onto the disc-condyle complex (Figure 12). Type II is encountered most commonly [14]. Some authors believe that internal derangement of TMJ is the result of LPM hyperactivity or hypoactivity, poor coordination between the two heads of the muscle, and/or a disturbance in the normal role of the muscle in control or stabilisation of the TMJ [15]. Because the upper head of the LPM attaches only to the capsule and disc in types I and III and does not attach to the condyle, from the anatomical perspective, it is possible for the upper head of the LPM to pull the disc forward independently of the condyle and hence predispose to disc displacement as well as prevent reduction of a displaced disc. A few studies have demonstrated that type I attachment is more commonly seen with DDwoR [16,17]. The LPM may prove to be a target for potential therapies (e.g. botulinum toxin injections), which could improve the management of this disorder [17].
III. Joint effusion
Joint effusion is also a commonly observed finding, most often in the superior compartment. Joint fluid represents an inflammatory response to a dysfunctional disc–condyle relationship [18]. Most often it is observed in the superior joint compartment; however, inferior compartment or both compartment effusion is also seen. Joints with effusion have been shown to more commonly have DDwoR rather than DDwR/wpR [11]. The presence of joint fluid (joint effusion) is seen as high signal intensity in the joint space on T2W images (Figure 13).
Figure 11
Posterior attachment remodelling. Sagittal oblique T2W-FS (A) and proton density fat saturation (B) images demonstrate normal posterior attachment (yellow arrow). In two different patients with long-standing internal derangement (C, D), sagittal oblique T2-FS images show a hypointense signal in anterior part of posterior attachment (PA) suggesting fibrosis (remodelling). In the second patient (D), this gives a pseudo-disc appearance
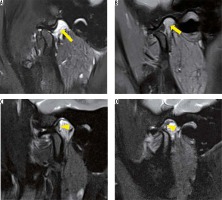
Figure 12
Types of lateral pterygoid muscle (LPM) attachments. A) Type I attachment. Sagittal oblique proton density fat saturation image reveals upper head of LPM (white arrow) inserting onto the disc and lower head (yellow arrow) inserting onto the condyle. B) Type II attachment. Upper head of LPM (white arrow) is inserting onto the disc and condyle. Lower head (yellow arrow) is inserting onto the condyle. C) Type III attachment. Upper head of LPM (white arrow) is inserting onto the disc while the middle head (yellow arrow) and lower head (blue arrow) are inserting onto the condyle
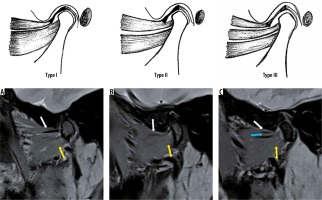
Figure 13
Ancillary findings – effusion, marrow oedema and capsular thickening. Sagittal oblique T2-FS images reveal effusion in the superior joint compartment (yellow arrowhead) (A) and bone marrow oedema (white arrowhead) (B) in two different patients. Coronal oblique (C) and axial (D) T1W images reveal marked thickening of joint capsule (yellow arrowheads) in two different patients
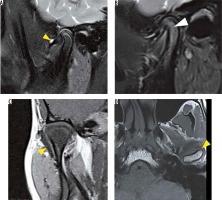
IV. Joint capsular thickening
Joint capsular thickening may also be observed. The joint capsule is assessed on coronal and axial T1W images (Figure 13). Capsular thickening is a common finding in joints with internal derangement.
V. Range of motion
Range of motion is assessed on T2 W Cine (dynamic MR) sequence. It is considered normal when the head of the condyle reaches below the articular eminence on open mouth position but not > 5 mm anterior to the crest of eminence. If it reaches far anteriorly and superiorly along the posterior slope of eminence, increased range of motion is recorded. If the condyle does not reach the crest of articular eminence, reduced range of motion is recorded. Increased range of motion is usually recorded with early DDwR, while reduced range of motion is characteristically seen in DDwoR.
Degenerative joint disease process
If stress to joints exceeds the biomechanical threshold, tissue breakdown occurs. This leads to osseous or ‘hard’ changes, which constitute degenerative joint disease.
Morphology of condyle, glenoid fossa, articular eminence, and joint space can be assessed on both CT and MR images. Bone marrow signal alteration involving the condyle or articular eminence is well assessed on MR. MDCT has been described in the literature as the imaging modality of choice for osseous changes in the TMJ. A multitude of osseous changes are seen in the course of the disease. Early changes include bone remodelling, which is seen as flattening (without loss of height), subchondral sclerosis, and volume loss of the condyle (Figures 14, 15). In joints with active DJD, erosions of the condyle are the most characteristic finding (Figure 16). As the repair phase sets in, these erosions get recorticated. Other findings include glenoid fossa and/or articular eminence irregularity, which are seen less commonly. Late changes include flattening with loss of height, osteophytes, and subchondral cysts [6] (Figure 17).
Figure 14
Flattening and subchondral sclerosis of condyle. Coronal oblique noncontrast computed tomography (NCCT) (A) and T1W (B) images of temporomandibular joint show normal thin cortical outline (yellow arrow) and convex articular surface of condyle. In a patient with internal derangement, coronal oblique NCCT (C) with corresponding T1W (D) images display flattening of articular surface with subchondral sclerosis as shown by thickened cortical outline (yellow arrowhead)
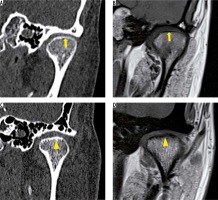
Figure 15
A-E) Regressive remodelling of condyle. In a patient with left-sided internal derangement, axial (A) and sagittal oblique (B, C) noncontrast computed tomography images show reduced antero-posterior dimension of left condyle (yellow arrow) with maintained vertical height suggestive of regressive remodelling. Right condyle shows normal volume (yellow arrowhead). Right axial T1W (D) and sagittal oblique proton density fat saturation (E) images in another patient with internal derangement show reduced condylar volume (yellow arrow)

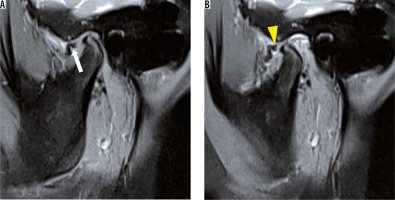
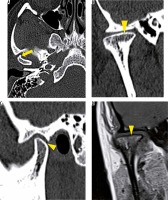
Figure 16
Erosions. In a patient with active erosive degenerative joint disease (DJD), axial (A) and coronal oblique (B) noncontrast computed tomography (NCCT) and sagittal oblique proton density fat saturation (PD-FS) (C) images show multiple cortical erosions (white arrowheads) with loss of condylar volume. In another patient with incomplete repair phase of DJD, sagittal and coronal oblique NCCT (D, E) and sagittal oblique PD-FS (F) images show loss of condylar volume and shallow concave erosions with a recorticated surface (yellow arrowheads)

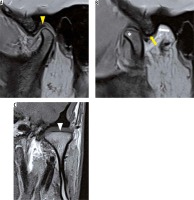
Figure 17
A-D) Osteophytosis and flattening with loss of height. In a patient with late stage of degenerative joint disease , axial (A), coronal oblique (B), and sagittal oblique (C) and T1W MR (D) images reveal osteophytosis (yellow arrow) and flattening of condyle with loss of vertical height (yellow arrowheads)
DDwoR has been found to be significantly associated with DJD findings like erosions and flattening with loss of height (p < 0.05), in various studies [19-21], suggesting that osteoarthritic changes are seen more commonly in joints with DDwoR. This supports the theory of sequential progression of ID-DJD.
Bone marrow oedema is a common finding encountered in patients with ID-DJD spectrum. T2W imaging has been found to be most accurate to determine marrow abnormalities [22]. However, STIR sequence can also be used for the same (Figure 13). Studies have shown that joints with bone marrow abnormalities are a subgroup of severe joint conditions and are significantly associated with DDwoR [11].
Joint space reduction is also a common finding in patients with ID-DJD. Joint space is assessed on sagittal and coronal oblique images.
There have been strong indications that bone changes in ID-DJD spectrum are more common in the condyle than in the remaining bone components of the TMJ [23,24].
Various studies have demonstrated very good agreement between CT and high-resolution MR imaging in delineating the above-mentioned osseous changes in TM joints affected with ID-DJD spectrum. Tasaki et al. [25] evaluated coronal and sagittal images of proton density and T2-weighted sequences of 55 joints in fresh cadavers and reported that the accuracy of MR in delineating the osseous changes was 93%. Alkhader et al. [26] conducted a study to determine the diagnostic accuracy of MRI for assessing osseous abnormalities of the TMJ with cone beam CT (CBCT) as the reference standard and found high specificity (84-98%) but relatively low sensitivity (30-82%). Their results showed that MRI was better at detecting changes in the size of the TMJ, such as deformities, than it was at detecting changes in shape, for example flattening, osteophyte formation, or erosion. They attributed this fact primarily to the limited spatial resolution of 1.5T MRI. In addition, when detecting osseous abnormalities in the articular fossa and eminence, difficulties sometimes arise due to magnetic susceptibility artefacts due to pneumatisation of these parts of temporal bone. However, improved spatial resolution of 3T MR has been shown to increase the sensitivity and specificity.
Utility of different magnetic resonance sequences
Certain imaging findings are picked up better on particular sequences on MR examination. T1W images best delineate the bone morphology, joint space, as well as anatomy of the structures surrounding the TM joints. Also, capsular thickening is best assessed on T1W coronal oblique and axial images. PD FS images best delineate the morphology, position, and signal of the disc. T2W FS images are helpful in assessing joint effusion as well as the morphology and signal of PA on open-mouth scans. T2W and STIR images best depict bone marrow signal alterations. T2W cine images are also acquired in most cases to have a real time assessment of the range of joint motion, which, when reduced, can have drastic effects on the feeding habits of these patients.
Hypermobile temporomandibular joints
TMJ hypermobility (also known as subluxation) is an overextension of the disc-condyle complex on opening beyond the articular eminence, and it is able to return to the glenoid fossa after either self-manipulation or spontaneous voluntary retention. There is a sudden forward movement of condyle during the latter phase of mouth opening and the condyle jumps forward beyond articular eminence to a wide-open position.
This condition is commonly associated with internal derangement of the TMJ. If, in addition to hypermobility, MRI shows findings of ID-DJD spectrum as well, it is possible to make more than one clinical diagnosis of TMD in such cases according to DC/TMD criteria [1,27].
Temporomandibular joint hypermobility has been found to be commonly associated with an anatomic variant in which the articular eminence has a steep (vertical), short, posterior slope and longer anterior slope. The maximum rotational movement of the disc is achieved before the maximum translation of condyle due to a steep eminence [27] (Figure 18). Other aetiological factors that have been implicated include connective tissue disorders like generalised joint hypermobility, Ehler Danlos syndrome and Marfan syndrome, iatrogenic trauma during dental extractions, intubation under general anaesthesia, endoscopic procedures, and sometimes intrinsic trauma due to yawning, wide mouth opening, seizure disorders, etc. [28,29].
Figure 18
Hypermobile temporomandibular joint. A) In a 25-year-old patient who presented with multiple episodes of open lock on left side, closed mouth sagittal oblique proton density fat saturation image reveals a normal disc (yellow arrowhead). B) Open mouth image shows increased range of motion where the condyle (asterisk) is seen reaching antero-superiorly to the crest of articular eminence (yellow arrow). Steep (vertical) posterior slope of AE (white arrow) is also noted. C) Coronal oblique T1W image shows flattening of condyle (white arrowhead)
The diagnosis is mostly made clinically as the patient presents with a history of a jaw “going out” when opening wide. Sometimes the patient reports clicking that is clinically audible as a “thud”.
Conclusions
We conclude that imaging has an important role to play in the diagnosis of internal derangement-degenerative joint disease spectrum affecting the TMJ. MR is an excellent imaging modality for the same. With its exquisite soft tissue contrast resolution, non-invasive nature, and multiplanar capability with no radiation hazard, MR is capable of demonstrating a broad spectrum of pathologies affecting the TMJ in great detail. MDCT is the standard modality for osseous changes in the TMJ. However, MR in various studies has shown comparable results in terms of osseous changes in internal derangement and hence can be a one-stop shop modality to evaluate the same.