Introduction
Foreign body implantation into soft tissues, either in the early period or late period, is a common cause of emergency department admissions. Infection, chronic pain, and fibrosis are frequent late complications in this patient group. Direct X-rays are preferred in the diagnosis of soft-tissue foreign-bodies (FBs) [1]. Some of the foreign bodies are visualized as radiopaque on direct X-rays; however, some radiolucent objects such as organic materials cannot be detected by direct X-ray examinations [2-4]. The visualization of an object on X-rays depends on not only its density, but also its size, location, and depth in the soft tissue [5]. Moreover, another disadvantage of direct X-ray examinations is ionizing radiation exposure [5]. Ultrasonography (US) is the second most preferred imaging modality in detecting FBs in soft tissue [5]. In addition to radiopaque materials, some radiolucent materials and the complications of these materials in the tissue can be determined without using ionizing radiation [2]. An important disadvantage of US is that it is a user-dependent modality [5]. However, showing soft-tissue FBs with high detection rates by an ionizing radiation-free method would be very useful in emergency departments.
In this study, we aimed to analyse the US detection rates for various sizes of foreign bodies placed in phantoms implanted into soft tissue.
Material and methods
Ethical approval
We conducted our study prospectively on phantoms. This prospective study was approved by the institutional review board of the Ethical Committee of our hospital.
Phantoms
Parallel to the long axes of the chicken pieces, a 1 cm deep slit was formed with a knife. A total of 740 pieces of chicken fillets 3 cm thick, 10 cm long, and 5 cm wide were prepared. A total of 20 pieces of glass, porcelain, plastic, wood, pencil-tip, chicken bone, iron, walnut shell, and fishbone, with a height and width < 0.5 cm and length < 1 cm, 1-3 cm, and 3-5 cm in rectangular shape were implanted into the slits opened in the chicken pieces, each on a separate chicken piece. In addition, 20 pieces of 1-3 cm long peanut shells, < 1 cm rose spikes, < 1 cm cactus spurs, < 1 cm pellets, and < 1 cm staples were implanted into chicken pieces separately. The chicken pieces were kept under light compression for 24 hours in order to remove air bubbles. No objects were placed in 100 chicken pieces. Each chicken piece was then placed separately in a latex glove. The latex gloves were filled with ultrasound gel and tied.
The imaging method
Sonography (Siemens, Acuson S3000, California, USA) was performed using a 5-14 MHz linear transducer.Each phantom was evaluated by a radiologist (7 years of experience) and an emergency medicine specialist (8 years of experience). The observers were blinded to the presence and kind of foreign bodies in phantoms. Examinations were carried out in 2 planes, in parallel with the long- and short-axis of the phantom, without time constraint. Each phantom was evaluated twice at 24-hour intervals.
Statistical analysis
The SPSS 20.0 program and Excel (Microsoft) were used to analyse the data. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated for each body considering the diagnoses of the 2 observers. The inter-observer compliance values were expressed using k statistics. A value of k equal to +1 implies perfect agreement between the 2 observers while that of –1 implies disagreement. If k assumes the value 0, then this implies that there is no relationship between the ratings of the 2 observers.
Results
Sensitivity, specificity, positive predictive value, and negative predictive value were calculated for each material. These findings are summarized in Table 1.
Table 1
Sensitivity, specificity, positive predictive value, and negative predictive value were calculated for each materiel
Significant differences were detected in the value of fish bones < 3 cm and > 3 cm of diagnostic value of US (p = 0.008 < 0.05). There was no significant difference between the diagnosis of US for < 3 cm and > 3 cm glass, porcelain, plastic, wood, pencil-type, chicken bone, iron, and walnut shell (p > 0.05); therefore, the diagnostic value of ultrasound is high in all sizes for these objects.
The kappa coefficient calculated for the inter-observer agreement was not statistically significant for < 1 cm glass, < 1 cm porcelain, < 1 cm plastic, < 1 cm wood, < 1 cm iron, < 1 cm fishbone, 1-3 cm fishbone, and 3-5 cm fishbone (p > 0.05). The kappa coefficient calculated for the inter-observer agreement was statistically significant for other FBs.
Discussion
On the sonographic examination of FBs implanted into the superficial soft tissue, the posterior shadowing or strengthening varies depending on the angle between the object and the probe. The posterior shadow becomes more prominent if the object and the probe are parallel to each other. Therefore, it is important to make a multiplanar evaluation. In our study, we performed 2-planar imaging. The smaller the size of the FBs, the more difficult it is to recognize them by US [6]. In this study, we evaluated the detectability of objects according to their dimensions. Comparison of different sizes are not available in the current literature.
In our study, the sensitivity, specificity, and accuracy were very good for the diagnosis of FBs. The sensitivity and accuracy were low for the cactus thorn. Cactus thorns may not be detected due to their thickness, as in our study.
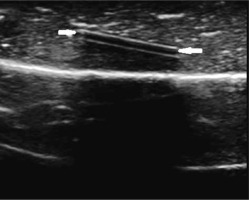
All the FBs examined in our study were hyperechoic (Figure 1). A hypoechoic line between the 2 hyperechoic linear lines was observed in the plastic FBs (Figure 2). We thought that this was due to the layered structure of plastic bodies formed during the production processes. Posterior strengthening was determined in FBs, which was more prominent in porcelain, walnut shell, peanut shell, and pellet.
Figure 1
A 1-3 cm glass phantom in pieces of chicken fillet on ultrasonography was hyperechoic (white arrow) with posterior acoustic shadowing
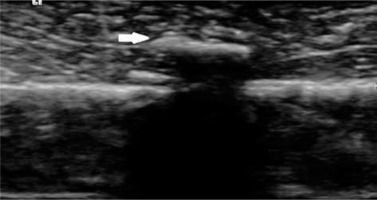
Figure 2
A plastic phantom in pieces of chicken fillet on ultrasonography, a hypoechoic line (white arrows) can be seen between the 2 hyperechoic linear lines
Detection and localization can be difficult with radiography. US, CT, and MRI are other methods for the evaluation of FBs. CT is ionizing radiation exposure. MRI is expensive [7].
There are many studies evaluating in-vivo and in-vitro detection of non-radiopaque FBs by ultrasonography. Bray et al. found that the sensitivity of US was 94% and the specificity was 99% in their study conducted with 1 × 4 mm and 2 × 5 mm sized wood, glass, and metal FBs implanted on the fingers of cadavers. They reported the sensitivity for small metals as 79%, 95% for small wood, 93% for small glass, and 100% for large wood and glass FBs implanted in the phalanges. When it comes to the FBs implanted in the palmar surface, the sensitivity was reported as 77% for small glass FBs and 100% for all other FBs [8]. Similarly to our results, US sensitivity increased as the size of the FB increased in this study. Many studies have been conducted with US on non-radiopaque objects, whereas none of these studies have evaluated the size of the FBs. In these studies, sensitivity and specificity values were found to be high for the detection of FBs by US.
In a study on phantoms by Driskell et al., radiologists and emergency medicine doctors evaluated phantoms in which 1 mm, 2 mm, and 3 mm wooden FBs had been implanted [8]. The sensitivity and specificity values were not different between the radiologists and emergency department physicians for the wooden FBs [9]. Similarly, in our study, there was a perfect fit between the results of US evaluation by the radiologist and emergency medicine doctors for the wooden FBs. But we also evaluated FBs other than wood, and there was no statistically significant difference between the observers for < 1 cm glass, < 1 cm porcelain, < 1 cm plastic, < 1 cm wood, < 1 cm iron, < 1 cm fishbone, 1-3 cm fishbone, and 3-5 cm fishbone.
Honton et al. reported that soft-tissue FBs appear hyperechoic on ultrasonographic examination [10]. In our study, all FBs were hyperechoic. In the case of a lack of strong posterior shadowing in the sonographic examination of FBs, muscle fibres may cause misinterpretations because they also cause hyperechogenicity on the US. In the distinction of these 2 conditions, following the muscle fibres longitudinally would be helpful.
In the study of Demiralp et al. on FBs in intraoral localization conducted with phantoms, they reported a hypoechoic halo around the FBs in the case of chicken bone fragment, root, stone, tooth enamel, amalgam, and orthodontic wire stab [11]. In our study, only the chicken bone fragment was examined among these FBs, and we did not observe a hypoechoic halo around it.
The phantoms created did not contain bone tissue. This was the main limitation of our study. Investigators in future studies may also wish to include a larger number of each individual FB to increase the power of the study. Because the study was designed in-vitro, we could not evaluate the findings such as fibrosis and inflammation occurring around the surrounding tissue in-vivo. We evaluated objects in a multiplanar fashion but did not evaluate in which plain they were better visualized. Furthermore, we did not use modern US techniques such as elastography, which was another limitation [12].
Finally, we only used a linear probe. Greater phantoms could be evaluated using a convex probe.






