Introduction
Critical limb ischaemia (CLI) is defined as ischaemic rest pain requiring regular use of analgesics, and nonhealing ulceration or gangrene of the foot or toes. Pain is a significant component in the presentation of patients with CLI. In most cases, pain is intolerably severe, and the control of pain is a critical aspect of the management of these patients [1-3]. Although opioids are widely used for the management of pain, they are often associated with dose-dependent, untoward side effects such as nausea and vomiting, sedation, somnolence, or possibly respiratory depression [4-7]. CLI occurs most frequently among the elderly population, who are most susceptible to the side effects of opioids and the risks of serious physiological complications. The prevalence of co-morbid conditions limited physiological reserve, cognitive impairment, and frailty in patients with CLI sometimes make it difficult to administer opioids to this population [1-8].
In recent years, there has been growing interest in identifying different analgesic options that are less opioid dependent [3-7,9]. Sciatic nerve block (SNB) is frequently used to induce anaesthesia for lower limb surgery around the knee, ankle, and foot [4-7,10-14]. It may be used to relieve acute pain emergencies, including distal lower limb fractures, and for postoperative pain control while waiting for alternative medications to become effective. Recent clinical studies have emphasised the use of SNB as an alternative method to improve pain management during endovascular treatment of CLI with severe rest pain [15,16]. They reported that SNB can be a useful tool to provide adequate analgesia and reduce the amount of opioids or anaesthesia required.
The management of pain is still challenging in patients with CLI because of frailty and poor tolerance. The analgesic strategy has to be efficient, with minimal side effects, and it must be easy to manage. There is a need to reduce the dependence on opioid analgesia, particularly during prolonged and complicated interventions. Thus, we evaluated the utility and efficiency of popliteal SNB anaesthesia/analgesia as an alternative method to relieve severe rest pain during endovascular treatment of CLI.
Material and methods
Patients
This study was approved by the Institutional Review Board and Ethics Committee. We conducted a retrospective evaluation of our clinical database to identify patients with CLI, who received US-guided popliteal SNB for the relief of severe rest pain during endovascular treatment of CLI. Each patient was evaluated by an anaesthesiologist and interventional radiologist for possible inclusion into the study, potential risk of complications, contraindications, or alternative anaesthetic techniques if required. All patients were thoroughly informed about the procedure, and written, informed consent was obtained from each patient. Exclusion criteria included any neurological dysfunction in the affected lower limb, cognitive or psychiatric dysfunction causing inability to comply with the study protocol, and allergy towards local anaesthetics or contrast media. The severity of CLI was evaluated according to Fontaine and Rutherford classifications. The definition of criteria for percutaneous management of CLI was based on reporting standards of Inter-Society Consensus for the Management of Peripheral Arterial Disease [1]. The presence of flow in the femoral, popliteal, dorsalis pedis, anterior, and posterior tibial arteries was routinely assessed with colour Doppler ultrasonography. Angiography was performed in each patient to plan the intervention, determine the nature and extent of the occlusion, and visualise the distal arterial tree in the affected limb.
Patient preparation and block procedure
The patients were connected to routine noninvasive monitors, such as electrocardiogram, blood pressure monitoring, and peripheral oxygen saturation. Intraprocedural complications including haemodynamic and respiratory changes were recorded. All patients were informed about the symptoms of local anaesthetic systemic toxicity, such as auditory/visual changes, lightheadedness, circumoral and/or tongue numbness/tingling, and metallic taste.
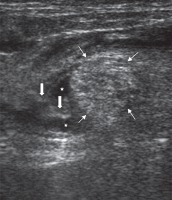
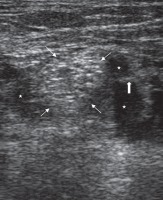
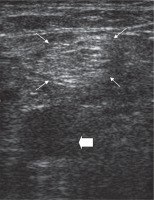
All patients underwent SNB prior to the angiography procedure. Each block was performed by an interventional radiologist (MG) who was experienced in US-guided peripheral nerve block. A posterior popliteal approach to SNB was employed in this study. The patients were placed in the prone position. After skin disinfection, an ultrasound system with a high-frequency linear transducer (9-13 MHz) was positioned to localise the sciatic nerve on the popliteal fossa. After identifying the sciatic nerve as a round, hyperechoic structure (Figure 1), the overlying skin was infiltrated with local prilocaine. A 21-gauge needle was inserted at a 45° to 60° angle to the skin and advanced slowly toward the target nerve in a plane from lateral to medial or medial to lateral direction (Figures 2 and 3). To avoid an incomplete nerve block, the needle insertion point was chosen just above the division of the sciatic nerve. After confirming that the tip of the needle was adjacent to the sciatic nerve, the block was conducted with multiple injections of local anaesthetic to create a circumferential spread around the sciatic nerve (Figure 2 and 3). In all patients, SNB was performed with a standardised mixture of 10 ml of bupivacaine 0.5%, 10 ml of lidocaine 2%, and 10 ml normal saline. The success of the block was defined as a significant relief of pain prior to endovascular treatment. If the patients were not satisfied with pain relief within five minutes, the block was repeated with the same dose of local anaesthetics. Narcotic medications were administered if required. The dose and time of administration were recorded.
Figure 1
Ultrasound image of the pre-injection sciatic nerve in the popliteal fossa. Thin arrows: sciatic nerve; Thick arrow: popliteal artery
Assessment of block performance and related pain
The degree of pain relief was graded by using subjective criteria from 1 to 4: 1 = no relief of pain; 2 = mild to moderate relief of pain; 3 = considerable relief of pain; and 4 = complete relief of pain. Patient and operator satisfaction with the pain management were evaluated and graded from 0 to 2: 0 = not satisfied at all; 1 = partially satisfied; and 2 = satisfied (very good or complete satisfaction).
Details of endovascular treatment, time to perform the block, amount of local anaesthetics, duration of block, need for supplemental analgesia, patient and operator satisfaction, and complications were recorded.
Results
Patients
In this study, 10 patients received US-guided popliteal SNB to relieve severe rest pain prior to endovascular treatment of CLI. The mean age of patients (seven males, three females) was 58.4 ± 13.1 years (range 29-86).
All patients were restless due to severe rest pain in the acute setting, and they were unable to lie on their back for a long time during endovascular treatment. Four patients were classified as stage IV of Fontaine (or category 5-6 of Rutherford) classification, which means all such patients suffered from more or less ulceration or gangrene. The remaining patients were stage III of Fontaine (or category 4 of Rutherford) classification, which means these patients suffered from ischaemic rest pain. All patients had symptoms including varying degrees of decreased temperature and pallor or a mottled appearance of the affected foot. Five patients had a partial sensory loss and motor deficit in their foot or fingers.
Two patients were recorded as undergoing amputation during the same hospital stay due to unsuccessful endovascular revascularisation. Four patients who had successful endovascular revascularisation received amputation within or after one month of initial endovascular treatment to stop ongoing gangrene or infection. One patient died within a week following endovascular treatment and another two patients in the next five years due to significant comorbidities.
Pain control and procedural parameters
In each case, SNB was technically successful, and all of the patients had complete resolution of the pain within five minutes. Pain relief did not exceed more than 12 hours. All patients were satisfied with the block anaesthesia, and no patient required additional analgesia in this period. The degree of pain relief was 3 in two patients and 4 in eight patients, after the administration of SNB. Time to perform the block was less than five minutes in each case. The amount of local anaesthetic necessary for adequate pain control was 20 ml of mixture (1 : 1 lidocaine/bupivacaine) diluted with 10 ml saline for each block.
In three patients, the pain was aggravated by distal migration of free-floating thrombus during thromboaspiration or thrombolysis. They required additional SNB the next day while waiting for the thrombolysis to become more effective. Two patients who required amputation after a failed attempt of revascularisation were supplemented with additional SNB for the following few days because of subsequent rebound pain. There was a 100% operator satisfaction rate with the pain control provided by SNB during endovascular treatment as well as after it for the first 12 hours. Operator comfort was also very good (100%) with regard to the prevention of unwanted patients’ leg movements during prolonged or complicated angiographic procedures. We did not experience any complications secondary to the nerve block.
Discussion
This study showed that US-guided popliteal SNB may provide adequate pain relief and thereby patient compliance allowing endovascular interventions to be performed without the use of supplemental analgesia. This technique may also provide a contribution to pain control in the next few days following initial endovascular intervention, while waiting for the thrombolysis to become more effective, or amputation if the revascularisation failed.
Various studies have demonstrated the benefits of SNB for pain control during or after painful procedures around the knee, ankle, or foot [4-7,10-14]. SNB may be a useful adjunct for certain lower limb chronic pain syndromes such as CLI [3]. The benefit of peripheral nerve block includes decreased pain, better patient satisfaction, reduced opioid consumption, and opioid-related side effects [4-7].
CLI is a severe stage of peripheral arterial disease. Patients with CLI can be classified in the grades of the Fontaine classification (stages III-IV) or the Rutherford classification (grades 4-6). The goals of management in patients with CLI are to relieve ischaemic rest pain, promote ulcer healing, prevent limb loss, improve patient function and quality of life, and prolong survival. Rest pain most typically occurs at night, but in severe cases it may be continuous. This results in sleep disturbance, causing a progressive decline of their physical and psychological state. Pain management is essential in improving function and quality of life. In most cases, the pain is intolerably severe, and it responds only to opioids [1-3]. Opioids are known to have a wide range of side effects that can result in suboptimal outcomes or serious life-threatening complications [4-7]. Patients with CLI have multiple co-morbidities, often including impaired renal function, diabetes mellitus, and advanced age. The use of high doses of opioids in these vulnerable patients may be limited because of untoward side effects or possible complications [1-8].
Ideally, relief of pain is achieved by reperfusion of the limb in patients with CLI [1,2]. Pain control may be urgently needed in these patients until revascularisation can be provided [1-3,9,15,16]. In severe cases, the pain occurs only after a short period of supine rest, and it may become impossible for the patients to lie on their back for a long time. On the other hand, endovascular treatment of CLI is a lengthy, painful, and uncomfortable procedure. Many patients with CLI exhibit symptoms of anxiety and poor compliance with prolonged revascularisation procedures. Moreover, they may have abnormal behaviour involving hyperactive or hypoactive psychomotor activity, disturbances of attention, or disorientation [1-3,8,15,16]. Although they may need effective pain control with higher levels of opioid medications during these interventions, they have poor tolerance to strong opioids. Doses should be balanced to keep the patient comfortable without substantial side effects. In severe cases, pain relief by the use of narcotic medications remains poor and the use of incremental doses can lead to the patient becoming restless, confused, and uncooperative. Changing the opioid-based analgesia should be considered if there is a poor response to pain or if dose-dependent side effects develope [1-8]. There has been much interest in recent years in identifying alternative analgesic approaches that are less opioid dependent [3-7,9]. Peripheral nerve blocks have emerged as options in the delivery of adequate pain relief in patients with CLI [3]. SNB may offer a solution to palliate severe pain while planning or during endovascular treatment of CLI. The achievement of a pain-free state without narcotic medications allows the patients to continue their cooperation with immobility in their leg during uncomfortable endovascular interventions. Therefore, nerve blocks may also provide a contribution to operator comfort during these complex and prolonged endovascular treatments [15,16].
The sciatic nerve can be blocked from several different locations along the lower limb. The popliteal fossa is the site where the sciatic nerve splits into its two major components: the tibial and common peroneal nerves. To block both components, either a single injection above the division of the sciatic nerve or two injections to block the tibial nerve and common peroneal nerve separately have been recommended [17,18]. Popliteal approaches to SNB were preferred from the posterior aspect of the leg with regard to the ease of performance of this approach under US guidance by via a high-frequency linear transducer. Bupivacaine and lidocaine were used concurrently, to combine faster onset of lidocaine and longer duration of bupivacaine [19]. Our study employed bupivacaine as a long-acting local anaesthetic, to ensure adequate intraprocedural and postprocedural pain control and anaesthesia.
Our study has several limitations. A potential limitation of this study involves the patient sample. The sample was based on available patients with CLI, who had restlessness caused by severe rest pain in the acute setting. The results of the study need to be confirmed in a wider patient population. Second, our results reflect a single interventional radiologist experience. The success of the nerve block is dependent on manual skills and experience, and therefore it is difficult to make a statement about the feasibility of this technique in clinical practice. Success rates may vary from clinic to clinic. Indications for SNB should be balanced carefully against possible complications or side effects and reserved for patients with serious comorbidities, who are unable to lie on their back for a long time during prolonged and complicated endovascular interventions. Third, the block resolution time did not record precisely because it was not considered as a primary objective in this retrospective study.