Introduction
Spondyloarthritis is chronic inflammatory, multisystem disease that affects the axial skeleton and mainly the sacroiliac joints (SIJs) [1]. Imaging of sacroiliitis has been the cornerstone in the diagnosis of spondyloarthritis. Features including subchondral bony erosion, bony sclerosis, narrowing of the joint space, and ankylosis are used for grading of sacroiliitis based on radiography according to the Modified New York Criteria (Table 1) [2].
Table 1
New York radiological grading criteria for sacroiliitis
While the diagnosis of early stages of axial spondyloarthritis depends upon the presence of inflammatory changes of the sacro-iliac joints, for late stages changes like subchondral sclerosis, bony erosions, and ankylosis are pathognomonic consequences for chronic inflammation [3,4].
Depiction of structural erosions in sacroiliac joints has great value in the evaluation of spondyloarthritis (SpA) because these erosions are an indicator of the severity, progression, and irreversibility of the disease [5,6].
Computed tomography (CT) provides high diagnostic capacity for the chronic inflammatory changes in SIJ spondyloarthropathy like erosion, but still with hazards of radiation, while magnetic resonance imaging (MRI) has the advantages of being the only imaging modality with diagnostic capacity for both active inflammatory and chronic structural changes [7,8].
Magnetic resonance imaging (MRI) STIR pulse sequence plays an important role in the depiction of bone marrow oedema in the active stage, while both CT and MRI T1 TSE sequence depict bony erosions; CT considered the gold standard because it has higher sensitivity and specificity [9]. Despite its higher diagnostic performance for erosion, CT is not routinely used in clinical practice due to its high radiation dose and its inferior capacity in depiction of bone marrow oedema in the active stage [9,10].
Routinely used MRI T1 TSE has restrictions that limit its diagnostic performance for the identification of bony erosions with indistinct boundaries between subcortical bone marrow and erosion, and also there is limited contrast separation between joint space and cortical space. As a result of these limitations there is a reduction in the sensitivity of erosion detection by T1 TSE [10].
Newly developed three-dimensional (3D) MRI sequences are gradient-echo (GRE) sequences provide high contrast between cortical bone, cartilage, and joint cavities, and help to provide images in different axial, coronal, and sagittal planes as reformatting datasets can be done any orientations. These newly developed sequences, in addition to the valuable soft-tissue contrast, cause no radiation exposure, and this plays a crucial role in the depiction of bony erosions [11].
These sequences, like the VIBE sequence from Siemens (volume interpolated breath-hold examination) and the THRIVE sequence from Philips (T1-weighted high-resolution isotropic volume examination) are fat-saturated 3D GRE sequences with short acquisition times, near isotropic resolution, and high image quality [12].
The aim of the work is to determine the diagnostic performance of the 3D MRI sequence THRIVE (T1-weighted high-resolution isotropic volume examination) in the depiction of structural erosions in sacroiliac joints in spondyloarthritis compared with the routinely used T1 TSE pulse sequence with MRI sequence zero echo time (Zero ET) as the standard reference.
Material and methods
Patients
This prospective study was approved by the Institutional Review Board (IRB), and informed consent was obtained from each patient before performing the MRI examinations. Between November 2021 and February 2023, 90 patients who underwent an MR examination were included in our study according to the following inclusion criteria: patients who had chronic low back pain for a period not less than 6 months and were suspected of having spondyloarthritis by the outpatient clinic rheumatologist. Fifteen patients were excluded, and the exclusion criteria were as follows: pregnancy, previous metallic devices, patients who had had a previous surgery, and patients with artifacts on MRI examination, e.g. motion artifacts. Finally, 75 adult patients (36 males and 39 females) were included in our study with a mean age of 44 years, (range 32-67 years).
Magnetic resonance imaging
Magnetic resonance imaging examinations of both sacroiliac joints were done using a 1.5 Tesla scanner (Ingenia; Philips Medical Systems, Best, The Netherlands) by using a transmit/receive body coil. The patients were in supine position, and T1 TSE, STIR, 3 D THRIVE, and zero ET sequences were obtained in both semi-coronal and axial images. Both THRIVE and zero ET sequences are 3D sequences added to the previously routinely used T1 TSE and STIR sequences. Table 2 shows the imaging protocols.
Table 2
Magnetic resonance imaging pulse sequences used in this study
After performing the MRI examinations for all patients, images obtained were studied and compared separately and independently by 2 radiologists with musculoskeletal experience without clinical information from the rheumatologist or laboratory examination results. The radiologist (reader 1) with 10 years’ experience assessed both sacroiliac joints for active inflammatory changes and structural abnormalities (erosions, sclerosis) on MR images while the other radiologist (reader 2) with 8 years’ experience assessed the MR images of the sacroiliac joints to test the inter-reader reliability.
Active inflammatory changes were diagnosed by the presence of high signal intensity on STIR images on either side of both sacroiliac joints, and cortical bony erosion was defined as loss of dark cortical signal and bony defect at the joint margin of the subchondral cortex of the iliac or sacral bone on T1 TSE and 3D THRIVE images, zero ET images were the standard reference to erosion identified on T1 TSE and 3D THRIVE sequence, and erosion on zero ET sequence was defined as bony defect of the subchondral cortical bone (Figures 1 and 2).
Figure 1
A 39-year-old male patient with chronic low back pain for 2 years with MRI of the sacroiliac joints, each row represents T1 TSE, 3D THRIVE, and zero ET, respectively. First row – coronal images, second row – their magnified view, third row – axial images, and fourth row – their magnified view. There are areas of subchondral erosions seen in iliac and sacral bones of left sacroiliac joint. These erosions are not clearly seen in T1 TSE and are well depicted in 3D THRIVE images (open arrow) and in zero ET (CT-like images) (arrows)
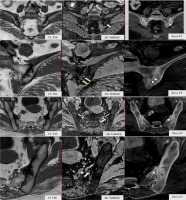
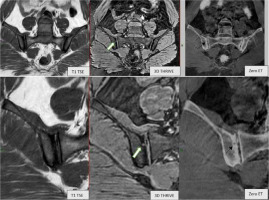
Figure 2
A 47-year-old female patient with chronic low back pain for 8 months with MRI of the sacroiliac joints. Each row represents T1 TSE, 3D THRIVE, and zero ET, respectively. First row – coronal images, second row – their magnified view. There are areas of subchondral erosions seen in iliac and sacral bones of left sacroiliac joint. These erosions are not clearly seen in T1 TSE and are well depicted in 3D THRIVE images (open arrow) and in zero ET (CT-like images) (arrows)
Scoring for erosions was performed according to their MRI appearance from 0-3 per region: 0 for negative (no erosions depicted), 1 for erosion size < 3 mm, 2 for erosion size 3-5 mm, and 3 for size > 5 mm.
Results were obtained, considering a false negative result if there was underscoring of erosion and a false positive result if there was overscoring.
Statistical analysis
The sensitivity, specificity, and accuracy of T1 TSE and 3D THRIVE sequences were calculated for both readers with zero ET sequence standard of reference. Values were calculated for erosions at both sacroiliac joints, and multiple comparisons of sensitivity, specificity, and accuracy differences were performed using Cochran’s Q. Cohen’s κ test was used to assess the inter-reader reliability of positive findings, and κ statistics were taken upon the base of Landis and Koch [13].
Statistically significant p values were considered if p < 0.05, and analysis was performed by using the software package SPSS 19.0 and 24 (Chicago, III).
Results
The mean age of the patients in the study was 44 years (range 32-67 years) with mean duration of chronic back pain of 2 years and 9 months (range, 6 months to 8 years). Forty-nine patients were HLA-B27 positive (65.3%). Fifty-six patients (74.6%) were diagnosed with spondyloarthropathy by an expert rheumatologist.
A total of 120 from 75 patients had subchondral bony erosions at the level of sacroiliac joints. The sensitivity and accuracy of 3D THRIVE for depiction of bony erosions was higher than that of T1 TSE (all p < 0.05), while regarding specificity no statistically significant differences were found between the 2 pulse sequences (all p > 0.05).
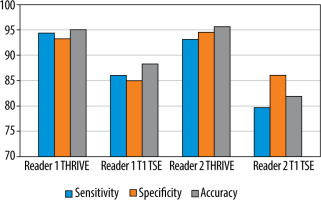
Accuracy, sensitivity, and specificity of 3D THRIVE and T1 TSE MRI sequences are summarized in (Table 3). The diagnostic sensitivity, specificity, and accuracy of 3D THRIVE were higher than those of T1 TSE for reader 1 (sensitivity: 94.5% vs. 86.2%; specificity: 93.4% vs. 85.1% and accuracy 95.2% vs. 88.5%) and for reader 2 (sensitivity: 93.3% vs. 79.9%; specificity: 94.7% vs. 86.2% and accuracy 95.8% vs. 82.1%) (Figure 3).
Discussion
Computed tomography scan was the gold standard for depiction of chronic structure changes like erosions of the sacroiliac joints more than 30 years ago [14]. Reporting of erosions increased in the last decade, using MRI in the diagnosis of sacroiliac osteoarthritis with the routinely used T1-weighted sequences [7]. In comparison with CT, MRI also has the advantage of detecting early inflammatory changes by using STIR pulse sequences, which is lacking in CT scans. Also, it has the advantage of reaching the diagnosis of early and chronic changes without radiation; hence, MRI is generally preferable and routinely used in diagnosis of chronic inflammatory spondyloarthropathy [1,15].
Recently used novel MRI sequences like VIBE and THRIVE sequences, which are a 3D T1 FAT SAT sequence, which result in thinner image slices, and which in turn leads to a high spatial resolution in the depiction of tissue abnormalities especially in cartilage [16].
In this study we compared the three-dimensional MR technique (THRIVE) with the routinely used T1-TSE sequence using the zero ET sequence as the standard reference for the depiction of erosions in the sacroiliac joints. Zero ET was used as reference instead of CT because it renders CT-like images without radiation hazard to the patient.
In our study, regarding the sensitivity of the 2 sequences, the 3D THRIVE sequence was higher than T1 TSE, i.e. 94.5% in 3D THRIVE and 86.2% in T1 TSE by one reader and 93.3% in 3D THRIVE and 79.9 % in T1 TSE by the other reader. Also, the accuracy of 3D THRIVE was higher than that of T1 TSE as it was 95.5% and 88.5%, respectively, by one reader and 95.8% and 82.1%, respectively, by the other one (Figure 1).
We found that 3D THRIVE sequence had higher sensitivity for detection of erosion than that of T1 TSE without a decrease in specificity. The 3D THRIVE sequence depicted significantly more erosions than T1 TSE when erosion counts were analysed by the 2 readers using the zero ST pulse sequence as a gold reference standard. The 3D THRIVE sequence was also superior to T1 TSE in terms of inter-reader reliability. The reader’s overall diagnostic accuracy for depiction of bony erosions was significantly higher using 3D THRIVE sequence than T1 TSE, which was more reliable in the depiction of erosions in the sacroiliac joints, which can help in better diagnosis of spondyloarthropathy together with clinical and laboratory findings.
Recent studies explored the evaluation of osseous structures using CT-like images derived from MRI scans like zero echo time. Breighner et al. [17] evaluated the role of these MRI images, which are like CT images based on the zero echo time sequence, which has good agreement with CT of the hip; hence, in our study we implemented the use of the zero ET pulse sequence as a reference standard between 3D THRIVE and T1 TET sequences instead of CT because it has the advantage of not exposing the patient to radiation.
Prior studies have evaluated the role of novel MRI sequences in the depiction of sacroiliac erosions. Diekhoff et al. [12] and Baraliakos et al. [10] assessed 3D volumetric interpolated breath-hold examination (VIBE), which is a gradient-echo sequence similar to 3D THRIVE. They found that 3D VIBE has a higher sensitivity in comparison with T1-weighted MRI in the detection of sacroiliac joint erosions without a loss of specificity. These findings are in keeping with our results regarding 3D THRIVE.
Our study had some limitations. All participating patients were referred from the Rheumatology Clinic, which may represent mild selection bias because there was no healthy individuals control group scanned for comparison. Also, there is no comparison between the diagnostic performance of the 3D THRIVE sequence and that of the zero ET sequence in the current study; further studies may be needed regarding this.
From the practical point of view, with its high diagnostic value and short time of about 3 minutes, the addition of the 3D THRIVE sequence to the routinely used MRI protocol for sacroiliac joint is highly recommended, which routinely includes T1 TSE and STIR short-tau inversion recovery sequence, because it improves the detection of structural changes and erosions. 3D THRIVE is a reasonable sequence for daily routine practice together with T1 TSE sequence, as both were found to have higher sensitivity in the depiction of articular changes and bony erosions in both sacroiliac joints in patients with spondyloarthropathy.
Conclusions
In conclusion, the 3D THRIVE sequence had higher diagnostic efficacy than the routinely used T1 TSE for the depiction of erosions in sacroiliac joints in patients with spondyloarthropathy. It is highly recommended that it be added into the routinely used MRI protocol in such cases, to improve the diagnostic sensitivity and accuracy in the depiction and evaluation of chronic structural changes in those patients.