Introduction
Over the past decade, the prevalence of obesity, particularly morbid obesity, has significantly increased, posing a considerable challenge for healthcare systems worldwide [1,2]. This growing health problem, marked by a rise in individuals with grade III obesity (a body mass index [BMI] equal to or exceeding 40 kg/m2), results in numerous comorbidities and places an increased strain on medical resources [2]. In individuals with morbid obesity, the execution of numerous diagnostic procedures, including computed tomography (CT), magnetic resonance imaging (MRI), and endoscopies, can be severely impeded or rendered infeasible [3]. The limitations stem from factors such as patient size exceeding equipment capacities, suboptimal image quality due to increased adipose tissue, and heightened procedural risks [3,4]. Consequently, these diagnostic challenges create significant barriers to timely and accurate identification of underlying medical conditions, thereby exacerbating the complexity of managing the health of patients suffering from morbid obesity. There are few studies about availability of CT, MRI, and endoscopy for individuals with morbid obesity [5].
We aimed to analyse accessibility of CT, MRI, and endoscopy procedures for people with extreme obesity in a significant sample of facilities in the Polish public healthcare system.
Material and methods
According to our university’s ethics committee, survey studies do not necessitate approval, and this study adhered to these guidelines. Furthermore, the research did not violate the principles outlined in the 1964 Helsinki Declaration.
Data collection
We conducted a telephone-based survey targeting CT, MRI, and endoscopy departments. We extracted details of hospitals providing CT, MRI, or endoscopy procedures using the Polish National Health Fund (pl. Narodowy Fundusz Zdrowia, NFZ) application programming interface (API) [6]. In November 2022, we identified a total of N = 2068 healthcare facilities offering at least one of the following procedures: CT, MRI, or endoscopy.
Initially, MKa developed a preliminary questionnaire for data collection via the telephone survey. Three authors (AK, TW, and MKi) contacted 20 randomly selected healthcare facilities to assess the feasibility of this initial questionnaire. Following the pilot telephone surveys, AK, TW, and MKi provided feedback on the questionnaire’s utility. MKa then refined the survey, which was subsequently approved by all authors.
The final questionnaire incorporated details about the healthcare facility obtained from the API, the number of telephone calls made, indications of successful calls, maximal weight and diameter capacities for CT and/or MRI, maximal weight capacity for endoscopy tables, information regarding whether the facility was located in a city with a population exceeding 100,000, details on whether the facility was an academic hospital, information on the presence of an emergency department at the facility, and details on whether CT, MRI, or endoscopy procedures could be privately obtained at the facility, paid out of pocket. If healthcare facilities possessed one or more of the devices analysed, we documented the highest capacities available at that particular facility.
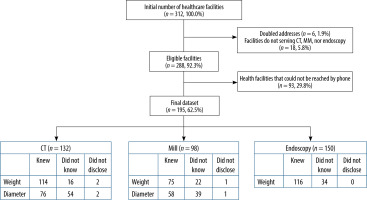
Data collection was performed between December 2022 and April 2023. MKa randomly selected a total of 312 healthcare facilities, representing 15.1% of the facilities listed in the NFZ API (Figure 1). Each of the 3 investigators (AK, TW, and MKi) made phone calls to 104 facilities. We excluded from further analysis any records that were duplicated in the NFZ resources, as well as facilities that, upon contact, stated they did not provide CT, MRI, or endoscopy services. If we were unable to establish contact with a facility after 3 phone calls (each made on different days during working hours), we excluded those records from further analysis. If the personnel were either unaware of or unwilling to disclose the capacities, we recorded that information in the form.
Figure 1
Flowchart presenting data collection process and distribution of answers in the final dataset
Both Grammarly and ChatGPT were used to rectify grammar and spelling errors in the text.
Data analysis
In the initial phase, we undertook a descriptive statistical analysis to ascertain the number of facilities aware of the maximum weight their CT, MRI, or endoscopy tables could accommodate. Additionally, for CT and MRI units, we assessed the maximum patient diameter the scanners could handle.
In the subsequent phase, we executed another round of descriptive statistical analysis, this time focusing on the data collected from surveys. Following this, we employed the chi-square test to compare facilities that had knowledge of specific equipment and endoscopy table parameters and those that did not. The characteristics scrutinized in this analysis encompassed the facility’s location in a city with a populace surpassing 100,000, the facility’s designation as an academic hospital, the presence of an emergency department at the facility, and the facility’s provision of private CT, MRI, or endoscopy services. We conducted an analysis on a subset of healthcare facilities that were knowledgeable about their equipment specifications. In this subset, we compared facilities with capacities at or above the median to those with capacities below the median of the studied group. A p-value less than 0.05 was deemed statistically significant.
The dataset comprising eligible healthcare facilities (n = 288 records) is presented in Supplementary File 1.
Results
From the initial dataset comprising 312 healthcare facilities, we excluded 6 due to duplicate addresses and 18 that did not offer CT, MRI, or endoscopy services (Figure 1). Out of the 288 eligible facilities, successful calls were reported in 195 cases, constituting 62.5% of the initial dataset. The final dataset represented 9.4% (195/2068) of the facilities providing CT, MRI, or endoscopy services in the public health system from the initial list collected from the NFZ API. Within the final dataset of 195 healthcare facilities, we acquired information regarding 132 radiology departments with CT equipment and 98 with MRI equipment. Additionally, 150 out of 195 facilities possessed an endoscopy department.
Of the departments analysed, 114 out of 132 (86.4%) were aware of the maximum weight capacity of the CT scanner, 76 out of 132 (57.6%) knew of its maximum diameter, 75 out of 98 (76.5%) were familiar with the MRI scanner’s maximum weight, 58 out of 98 (59.2%) knew its maximum diameter, and 116 out of 150 (77.3%) were knowledgeable about the maximum weight for endoscopy (Figure 1).
The general characteristics of the healthcare facilities evaluated are presented in Table 1. Most of these facilities were situated in cities with populations fewer than 100,000 residents. Approximately half of the facilities were equipped with an emergency department. Likewise, about half of the studied facilities provided private CT, MRI, or endoscopy services.
Table 1
General characteristics of the analysed healthcare facilities. Percentages represent the fraction of the total number of records in the final dataset (n = 195)
We found that facilities knowledgeable about the maximum diameter of CT scanners [facilities providing CT maximal diameters: 64 (82.4%) perform CT privately vs. facilities not providing CT maximal diameters: 36 (64.3%); p = 0.015] and MRI’s maximum weight [facilities providing MRI maximal weight: 63 (82.0%) perform MRI privately vs. facilities not providing MRI maximal weight: 13 (56.5%); p = 0.013] more often provided private CT/MRI services (Supplementary Table 1). Analogous trends were discerned for MRI maximum diameter and the maximum weight for endoscopy concerning private endoscopy services. We noted that healthcare facilities from cities with populations surpassing 100,000 more frequently reported higher CT maximum weight capacities [lower median: 7 (19.4%) vs. higher or equal to median: 30 (38.5%) facilities located in cities with over 100,000 residents; p = 0.072] (Supplementary Table 2). Nevertheless, no further associations between device capacity limits, city population, academic status of the hospital, presence of an emergency department, and the option to undergo private diagnostics were identified.
Discussion
In our study, we conducted a telephone survey to assess the maximum weight and diameter capacities of CT, MRI, and endoscopy tables in Polish facilities that perform these procedures in the public healthcare system.
Main findings
A Polish epidemiological survey in WOBASZ II recorded that, during 2013-2014, grade III obesity was present in 1.2% of adult males and 1.9% of adult females living in Poland [7]. In certain provinces, this percentage reached as high as 3-4% of the population. Rulkiewicz et al. estimated that among Polish working adults during 2016-2020 the percentage of those with extreme obesity (BMI ≥ 40 kg/m2) ranged between 0.7% and 0.9% [8]. Given that grade III obesity often leads to health issues and disabilities, this implies that such patients are less likely to be professionally active, and hence the current prevalence might be even higher than recorded in the study [8]. However, neither of these studies provided a distribution of body weights of the studied population.
To our best knowledge, our investigation is pioneering in Poland and is among the few globally to address the real-world availability of CT, MRI, and endoscopy for patients of extreme weight. Ginde et al. reported that in the first decade of the 21st century, only 11-28% of American hospitals could perform CT scans on patients weighing over 450 pounds (approximately 204 kg) [5]. For MRI, this percentage was even smaller, ranging from 9 to 10%. Presently, in Poland, the availability of CT for individuals weighing over 200 kg appears to be superior to that reported by Ginde et al., but the accessibility to MRI for the same weight is worse in our report [5]. Regrettably, we could not identify additional studies estimating the maximum capacities of imaging and endoscopy units in different countries.
Our analysis revealed that personnel in facilities offering both public and private CT or MRI services were more frequently familiar with the maximum diameter permissible for CT and the weight limits for MRI patients. A similar trend, albeit not statistically significant, was observed for endoscopy. We hypothesize that these centres handle a greater volume of imaging requests, and patients seeking private services often inquire about the capacities of the equipment in these facilities. We also identified a trend indicating that CT devices with larger patient capacities were primarily located in larger Polish cities with populations exceeding 100,000 inhabitants. This trend is probably due to the cost-effectiveness for larger hospitals in bigger centres to invest in equipment capable of accommodating patients with extreme obesity.
Strengths and practical implications
Our study’s strengths lie in its large sample size; we managed to gather data from approximately 9% of the facilities providing imaging or endoscopic procedures performed in Polish public healthcare system. We highlighted that the staff were often unfamiliar with the maximum capacities of the equipment they operated. Furthermore, slightly over a quarter of CT units could accommodate patients weighing over 200 kg, whereas for MRI this was restricted to approximately 5%. Almost 40% of endoscopy units met this criterion. Our findings underscore the tangible barriers extremely obese patients face, especially when advanced imaging diagnostics like MRI are required.
Limitations
The study has several limitations, mainly related to the telephone survey methodology. Firstly, our dataset has many missing data points, which may arise due to nonresponse or incomplete information from respondents. Secondly, the reliance on self-reported data may introduce response bias, compromising the accuracy and generalizability of the findings. Finally, the cross-sectional nature of the survey restricts the ability to establish causal relationships or assess changes over time.
Conclusions
In conclusion, a significant proportion of Polish facilities providing CT, MRI, and endoscopic examinations in the Polish public healthcare system were unaware of their equipment’s weight and diameter limits. Merely 5% of the surveyed MRI facilities could potentially accommodate a patient weighing over 200 kg.






