Introduction
Back pain is one of the most common reasons for adult patients to see a doctor, both in primary care and in emergencies. Nevertheless, among paediatric patients, non-traumatic back pain is often underestimated by both caregivers and physicians of various specialties. Contrary to popular belief, back pain is a relatively common symptom in children and adolescents. Common causes include muscle strain or spasms, spinal deformities (e.g. Scheuermann’s kyphosis, juvenile idiopathic scoliosis), birth defects – spondylolysis, bulging or herniated discs, and spondyloarthropathies such as ankylosing spondylitis. These causes can manifest as low back pain and stiffness, and they often get worse in the morning. Less common but more serious causes include malignancies and infections, such as common appendicitis, pneumonia, and rarely pancreatitis [1-3].
The aim of the study was to present the results of magnetic resonance imaging (MRI) of the spine in paediatric patients referred for examination due to pain and other non-specific clinical symptoms. Back pain was the leading cause of 1/5 of referrals to the MR laboratory after excluding other objective causes based on the interview. The list of diseases causing back pain is not exhaustive. Still, it reflects the pathologies and disorders among young children and adolescents diagnosed during 3 years in the radiology department of a tertiary paediatric hospital, ranging from sports injuries to fatal cancers.
Material and methods
The radiological documentation was included in the retrospective analysis. The MRI examinations carried out in 2020-2022 at the Department of Paediatric Radio-logy were re-evaluated. Medical records of 328 children referred for spinal MRI were reviewed. The criterion for inclusion in the analysed group was back pain. In 20% of referrals for MRI examinations, i.e. in 68 patients, pain in the area of the spine, the so-called back pain in the cervical, thoracic, or lumbar region was one of the leading clinical symptoms. Gait, muscle weakness, or sensory disturbances in the arms or legs have also been reported as associated symptoms. Some patients presented a forced position with the abolition of physiological curvatures of the spine. The final analysis included 68 patients aged -17 years. The criterion for inclusion in the group assumed that this was the first MRI examination performed on a patient.
The remaining 80% of spinal MRI examinations in 260 paediatric patients were performed for other non-pain-related reasons. Radiographic images of patients referred for post-injury diagnostics, supplementary assessment in oncology patients with a primary CNS tumour, and in children with suspected or already diagnosed defects were excluded from the analysis, e.g. myelomeningocele, including patients before and after surgery. Ten per cent were children referred due to bedwetting or loose stool, in order to exclude lumbar spine defects.
The examination was performed with a 3T Magnetom Spectra (Siemens Healthcare Germany) using a 20-channel head/neck coil or a 24-channel spine coil. In the case of suspected tumour or inflammatory changes the gadolinium contrast agent was administered intravenously using an automatic syringe based on body weight (V = 0.1 mmol/kg b.w.).
The tests were analysed on two-monitor diagnostic stations with the use of the integrated syngo.via system. The studies were reviewed by 2 paediatric radiologists with more than 10 years of experience. Patients were referred to the study by paediatricians, specialists in neuro-logy, rheumatology, and paediatric surgeons.
The spine MRI protocol implemented in the patients studied is shown in Table 1.
Table 1
Magnetic resonance imaging (MRI) sequences
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Results
In 68 patients with back pain as the first diagnosis, 53% (36 patients – 16 girls and 20 boys) showed abnormalities. The rest of the tests were assessed as normal. Bone and ligament elements, as well as the canal, spinal cord, and spinal nerves, were analysed. The decision to administer the contrast agent was made by the radiologist.
Among the patients with an abnormal MR image, the largest group were children with degenerative changes dia-gnosed: 10 children (28%) aged 13-17 years, including 8 girls and 2 boys. Perineuronal cysts were diagnosed in 2 girls (5%) aged 12 and 17 years, in a 4-year-old girl, and a 14-year-old boy (5%), and excessive kyphosis combined with scoliosis was diagnosed as the cause of the ailment.
In 9 patients (25%) the final diagnosis qualified the patients to the group of oncological diagnoses. The study showed, among others, the presence of neuromas; the final diagnosis in these patients was neurofibromatosis (NF1). There were also cases of a tumour with a final diagnosis of neuroblastoma, a tumour in the course of lymphoma, leukaemia (AML), or histiocytosis. In this group of 6 boys and 3 girls, the age of the patients varied greatly, from 2-16 years.
Another group of 7 (19%) patients, 6 boys and one girl, aged 6-14 years, were children diagnosed with inflammation, including Guillain-Barré syndrome, demye-linating changes in the course of ADEM, and inflammation in the course of tuberculosis.
The last group of 5 patients, 4 boys and one girl aged 3-17, presented symptoms most likely related to the trauma, including overload changes in a girl practicing rhythmic gymnastics – a thorough interview confirmed the potential risk of injury.
One 7-year-old boy was diagnosed with large calcifications within the intervertebral disc, which was the cause of persistent pain. Initially, X-ray and CT were performed.
All final clinical diagnoses presented by the authors, e.g. AML, ADEM, lymphoma, and others, were confirmed in laboratory or histopathological tests.
The cumulative results divided into groups are presented in Table 2. Examples of MRI images of patients from each group are shown in Figures 1-7.
Table 2
Demographic data and findings detected in MRI
Figure 1
Magnetic resonance examination of spine. PT3 – 14-year-old girl with disc herniation – arrow. A) T1-weighted sag, B) T2-weighted sag, C) T1-weighted axial, D) T2-weighted axial. A left-sided intraforaminal disc herniation at L3/L4 with suspected impingement of the left exiting L3 nerve
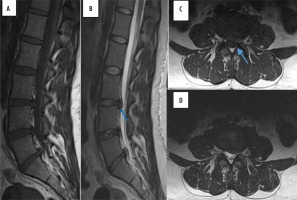
Figure 2
Magnetic resonance examination of spine. PT21 – 5-year-old girl with histiocytosis – arrow. A) T1-weighted sag, B) T1-weighted post contrast sag, C) T2-weighted sag, D) T2-weighted short time inversion recovery TIRM sag. Well-defined lesion in the central part of the L2 vertebra with a low-signal band visible in all sequences, slightly enhancing after contrast administration
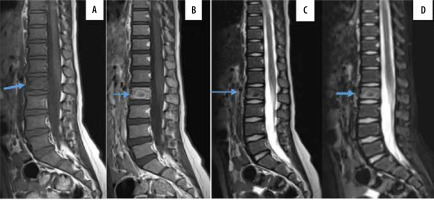
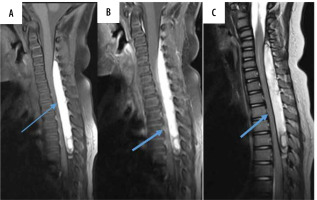
Figure 3
Magnetic resonance examination of spine. PT16 – 9-year-old boy with acute myeloid leukaemia, myeloid sarcoma – arrows. A) T1-weighted sag, B) T1-weighted post-contrast sag, C) T2-weighted short time inversion recovery TIRM sag. Multifocal mass of the tumour, enhancing after contrast administration, visible inside the spinal canal, epidural. Second lesion visible on the anterior surface of the sacrum
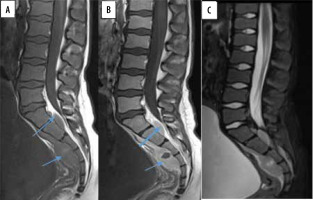
Figure 4
Magnetic resonance examination of spine. PT26 – 10-year-old boy with tuberculosis – arrow. A) T1-weighted sag, B) T1-weighted post contrast sag, C) T2-weighted sag, D) T2-weighted short time inversion recovery TIRM sag. Irregularity of both the endplate and anterior aspect of the vertebral bodies Th10-Th11, with bone marrow oedema and post-contrast enhancement. Complete destruction of the intervertebral disc

Figure 5
Magnetic resonance examination of spine. PT 27 – 12-year-old boy with acute transverse myelitis – arrow. A) T1-weighted sag, B) T1-weighted post contrast sag, C) T2-weighted sag, D) T2-weighted short time inversion recovery TIRM sag. Changes involve numerous segments of the spine, more than two-thirds of the cross-sectional area of the core with spinal cord enlargement. T1-isointense, T2-hyperintense signal, T1-post-contrast enhancement
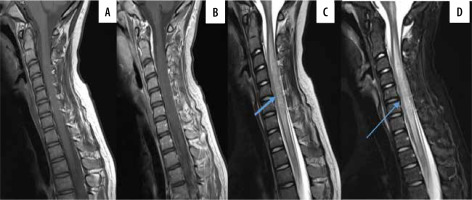
Figure 6
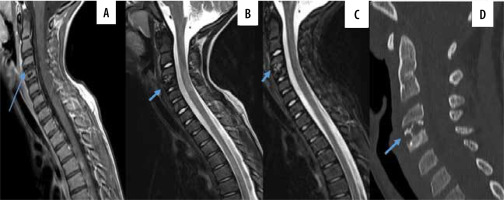
Magnetic resonance and computed tomography (CT) examinations of spine. PT 36 – 7-year-old boy with Iintervertebral disc calcification – arrow. A) T1-weighted sag, B) T2-weighted sag, C) T2-weighted short time inversion recovery TIRM sag, D) – CT MPR sag bone window. CT of the spine confirmed the presence of calcification. MRI of the cervical spine showed an altered signal intensity involving the intervertebral disc at C3-4 with areas of T1 and T2 hypointensity consistent with calcification
Discussion
The prevalence of back pain in children and adolescents varies widely, from 12% to 50% [3]. Back pain with other symptoms in children can be the beginning of a severe medical condition, but it is often neglected by caregivers as well as by doctors. This is due, among other things, to the fact that in the case of children, the cause of the ailment is not always found. Physical examination, including neurological assessment, is challenging in the youngest age group, and access to imaging tests, including MRI, is limited by the high cost and in many cases the need to anaesthetise the patient. In the case of the analysed group it was possible to determine the most likely cause of pain in 53% of cases. The results were similar to those of another author, who received a specific diagnosis in 52-73% of the cases [4].
There is no standard imaging work-up for back pain in children. Various algorithms have been used and are proposed for routine clinical practice. However, MRI imaging is increasingly being used as the first-line imaging technique when serious pathology is suspected in a child with back pain. It is possible to assess bone marrow oedema (visible e.g. in stress fractures) or to assess spondylolysis [5].
Osteoarthritis, disc herniation, spinal stenosis, and sacroiliac joint dysfunction are all part of the differentiation. Distinguishing the signs and symptoms of nociceptive (mechanical) pain from neuropathic pain (radiculopathy) is an essential first step in the diagnosis of back pain [6]. Lumbar disc herniation (LDH) is not a common condition in children. The overall incidence of LDH in children is unknown, and the diagnosis of LDH is usually delayed in children compared with adults [7]. In the evaluated group, in 10 children (28%), changes associated with disc degeneration, scoliosis, or the presence of Torlov cysts were diagnosed as the basis of pain. The role of the radiologist is important in making the final diagnosis. A precise description of the examination, taking into account anatomical variants and differences resulting from the patient’s age and unfinished growth, allows the patient to be qualified for conservative treatment, rehabilitation, or surgery.
Malignant causes of low back pain in childhood may be benign and involve the bones (e.g. osteoma, osteoblastoma, eosinophilic granuloma). The cause may be primary malignant tumours (Ewing’s sarcoma, osteosarcoma), metastatic cancers, or histiocytosis. We should also remember less typical ones, such as leukaemia and lymphoma. Spinal cord tumours constitute a separate group [8-10]. Back pain can be classified as spinal pain (70%), root pain, and tract pain. Spinal pain is characterized as a dull and aching pain localized to the bone segments adjacent to the tumour. Spinal pain is also believed to result from focal distension of the dural sack by the tumour. Root pain may mimic pain resulting from disk herniations. In the evaluated group, 25% of the probable causes of back pain were oncological changes in 9 patients. In this group, both vertebral body destruction and the presence of paraspinal or extramedullary tumours were noted. Paravertebral malignant tumours constitute 4.8% of cancer cases in paediatric oncology and are mostly composed of neuroblastoma (46.4%) and soft tissue sarcomas (35.7%). As in other cases, one of the basic symptoms next to neurological disorders is back pain [11,12]. Persistent pain, gait disorders, and neurological symptoms, especially in the youngest age group, should lead to deeper diagnostics. Delayed diagnosis can cause neurological deficits, almost resulting in permanent disability.
The inflammatory background in the presented material comprised the third most numerous group. Probably, in cases where neurological symptoms dominated rather than back pain, it was the most common diagnosis. However, in the presented study, back pain was the leading symptom. In the above group, out of 7 children, 6 were finally diagnosed with diseases caused by an autoimmune reaction, most often in the course of another infectious disease, e.g. acute disseminated encephalomyelitis, transverse myelitis, or Guillain-Barré syndrome. In these cases, the suggestion of radiological diagnosis significantly shortened the diagnostic path. The diagnosis of tuberculosis came as a surprise. However, this should always be taken into account. Skeletal tuberculosis is diagnosed in almost 10% of patients diagnosed with tuberculosis, including tuberculosis of the spine, accounting for almost 50% of reported cases of skeletal tuberculosis [13,14]. Tuberculous spinal injury in children causes more damage because most of the vertebral bodies are cartilaginous. Early diagnosis is very important to prevent progressive spinal deformities [15].
The prevalence of back pain appears to be higher among young athletes compared to the general population of the same age, suggesting a causal relationship with competitive sport. Several factors seem to play a role, such as the type of sport or the intensity of physical training [16]. In the study group, 5 patients had an MR change that may be caused by injuries. Despite the lack of information about the direct injury, the children regularly practiced sports, which could have been the direct cause of the changes visible in the imaging tests. The suggestion made in the radiological diagnosis was the reason for repeating and making the medical history more detailed.
The last case presented is a rare change from the group do not touch lesions – paediatric intervertebral disc calcification IVDC. The aetiology of IVDC is unclear [17]. It is more commonly seen in males, and the cervical spine is the most common location where it is primarily symptomatic, as in our case. In this case, the radiological diagnosis made it possible to resign from the biopsy suggested by the neurosurgeon.
The study is limited by the small number of patients and the short observation period during the COVID-19 pandemic.
Conclusions
A review of the literature indicates that both the prevalence and incidence of back pain increases with age, including cases in children. According to some authors, the incidence of back pain is higher among boys, others believe that it occurs with the same frequency regardless of gender [18], as in the presented manuscript. Spinal pain, especially with accompanying neurological symptoms, should not be underestimated. Although in most clinical situations the MR image is normal, in the case of persistent symptoms and neurological abnormalities found by the clinician, it is necessary to consider extending the diagnostics with an MR examination, which can accelerate the correct diagnostic path or make a very precise diagnosis.