Introduction
The vermiform appendix is the most variable abdominal organ in terms of position, extent, peritoneal, and organ relations [1]. Knowledge of the variations in the position of vermiform appendix is important because in appendicitis, its variable positions may produce variable symptoms and signs, which mimic other diseases [2,3]. An adult appendix is a long diverticulum, averaging 10 cm in length that arises from postero-medial wall of caecum, approximately 3 cm below ileocecal valve at confluence of 3 taeniae [4,5]. The origin of vermiform appendix is relatively constant; however, the tip can present variable positions. Variations of the appendix position usually result from a complicated and changeable embryonic development of the cecum [6,7], and/or variable length of the appendix [8]. Different studies reported various prevalence of positions. The most frequent location of appendix has been a controversial issue; in several studies conducted on cadavers or during laparoscopic surgery, retrocecal [9], pelvic [10,11], or post-ileal [1] positions were the most common locations [12]. One of the studies on cadavers reported retrocecal as the most common position, followed by sub-cecal, post-ileal, pelvic, and para-cecal, making pre-ileal as the least common position [9]. Another study reported retrocecal (27%) as the most common position in males, and promonteric (36.4%) as the most common in females [13]. A study on 100 cadavers in a similar region to ours (Uttar Pradesh, India) reported retrocecal as the most common position (58%) [14]. These differences in positions are thought to be related to differences in lifestyle and genetic structure [13]. Ultrasonography and computed tomography are the main imaging modalities used in evaluation of the appendix. Continuing advancement of multidetector computed tomography (MDCT) technology with excellent spatial resolution and the use of reformatted images have made it possible to delineate the entire length of appendix, whether inflamed or normal as well as to provide clearer illustration of a relationship of the appendix to its adjacent intra-peritoneal structures [15].
Imaging with ultrasound and/or computed tomography (CT) is considered essential in the early diagnosis of acute appendicitis, particularly when the patient presents with unusual features. Variable anatomical location of the appendix contributes to multiplicity of presentations. Not only location, but also size of the appendix is equally important in diagnosing or excluding a pathology.
Despite the widespread use of CT for evaluation of appendicitis, only few studies exist in the published literature that have systematically evaluated normal appendix [16-19]. Computed tomography criteria for normal size and wall thickness were primarily based on data from the literature using ultrasound (US). This extrapolation of US findings of a normal appendiceal thickness is based on the size of collapsed appendix without considering the luminal content. On computed tomography, the normal appendix is less than 6 mm in diameter from serosa-to-serosa [20,21]. However, some studies consider 6 mm criteria with no peri-appendiceal inflammation inefficacious [22]. Various authors report 7 mm as the appropriate threshold for normal appendiceal diameter [21]. Wall thickness of less than 2 mm is thought normal [20]. The normal appendix may be filled with air or contrast material, whereas fluid-filled appendix may indicate pathology. In the present study, we aimed to estimate the frequency distribution of different anatomical positions of vermiform appendix in patients with non-appendicular symptoms, and to estimate the range and the mean of diameter, wall thickness, and length of appendix in these individuals.
Material and methods
This retrospective descriptive cross-sectional study was performed among patients, who had undergone computed tomography (CT) scan of abdomen for various non-appendicular signs and symptoms between 2020 and 2021. Data of these patients were collected from picture archiving and communication system (PACS) and hospital information system (HIS) of our institute. Patients in whom the appendix could not be identified (n = 173) or in whom various parameters were unmeasurable (n = 31) were excluded from the present study. Similarly, patients with non-appendicular signs and symptoms but showing appendicolith or other CT features suggesting some peri-appendiceal inflammation were also excluded from the study (n = 28). A total number of 1,575 patients constituted the sample size of our study, which was approved by our institutional ethics committee. No informed consent was required due to retrospective nature of the study.
All patients underwent CT scan of abdomen using Phillips Brilliance 64-slice computed tomography scanner. Bowel preparation of patients was done with 2 tablets of bisacodyl 5 mg the night before scanning, which was performed after at least six hours of fasting. A 1.5 liters solution of 3% mannitol with water was given to patients over 50 minutes time, and images were acquired with slice thickness of 5 mm using parameters as follows: 120 KV, 200-300 mAs, pitch: 1.078, gantry rotation time: 0.75 s, FOV: 300-400 mm, slice interval: 5 mm, scan time: 8.6 s, collimation: 64 × 0.625. A non-ionic dimer iodinated contrast, iodixanol (2 ml/kg), was administered to patients through intravenous route.
Appendix was evaluated by a radiologist with more than 12 years of experience in abdominal CT on a commercially available Phillips workstation (Philips Brilliance 64-slice CT system, version 6.4) using multi-planar reformations (MPR) in axial, coronal, and sagittal CT images. Advance vessel analysis (AVA) was applied to measure different parameters of appendix. After bone removal in vessel extraction mode, ‘Create new vessel’ tool was used to place seeds every other axial slice for real-time manual centerline creation. Next, by double clicking the created centerline, the course of appendix was generated along its entire length as a curved structure. Then, ‘Inspect and measure’ tool was used in ‘Quick inspection’ mode, and ‘Select and mark a finding’ tool was applied to measure length, diameter, and wall thickness of appendix. The dia-meter was measured in axial display in most prominent part of appendix, and the mean of two perpendicular measurements was recorded (Figures 1 and 2). Position of the appendix was assigned based on position of appendicular tip as follows [4,13]:
Retrocecal: Tip of appendix situated posteriorly and superiorly to the cecum or ascending colon.
Paracecal: Appendix located lateral to the cecum and ascending colon.
Sub-cecal: Under the cecum.
Pelvic or descending intra-peritoneal: Appendix directed inferiorly and pointing towards pelvis.
Pre-ileal and post-ileal: Tip located antero-superior or postero-superior to the ileum.
Promontoric: Appendix pointing below pre-ileal and post-ileal positions, but not pointing towards the pelvis.
Figure 1
Measurement of length of normal appendix on computed tomography. In the left side viewport path, the appendix was marked in axial images till end point by placing seeds marked by green line. In the top right side viewport, the appendix was visualized along its complete length as a linear structure. Length measurement was done by tracing this path starting from the base up to the tip of appendix, and measurements were available on the screen. In the bottom right side viewport, the tip of appendix, i.e., the end point of the created path, is visible in sagittal image (white arrow)
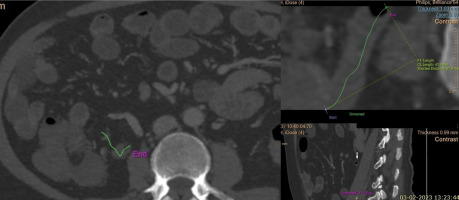
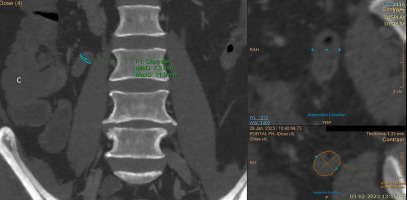
Figure 2
Measurement of diameter of normal appendix on computed tomography. After generating the path of appendix and clicking the diameter measurement tool, coronal images were displayed in the left side viewport, and the cursor was placed on the most prominent part of appendix. Next, the image truly perpendicular to the axis of appendix was identified, and measurement was made in axial display visible in the bottom right viewport
Data was analyzed, and percentage distribution of different variants of the appendix was calculated within the study population. Mean diameter and range of diameter of the appendix and wall thickness were measured with a calculation of mean and range of appendicular length.
Results
The total of 1,575 patients (age range, 18-87 years), who had undergone CT scan of abdomen for various non-appendicular complaints were included in the current study, out of these, 865 were males and 710 were females. The most common appendicular location was retrocecal (n = 400, 25.4%) (Figure 3), followed by sub-cecal (n = 320, 20.3%) (Figure 4), post-ileal (n = 295, 18.7%) (Figure 5A), and pelvic locations (n = 260, 16.5%) (Figure 6). Pre-ileal (Figure 5B) and promontory location (Figure 7) were found in 125 patients each (7.9%). The least common location was paracecal found in 50 patients only (3.1%) (Figure 7).
Figure 3
Contrast enhanced computed tomography image in (A) sagittal plane shows retrocecal appendix (arrow) lying behind the cecum (C). Coronal image shows the appendix lying in the retrocecal fat plane (B). Images (C) and (D) show sub-hepatic location (arrow), with tip lying on the undersurface of the liver

Figure 4
Contrast enhanced computed tomography images in coronal plane (A-C) show sub-cecal appendix (marked with arrow), with tip lying below the cecum (C)
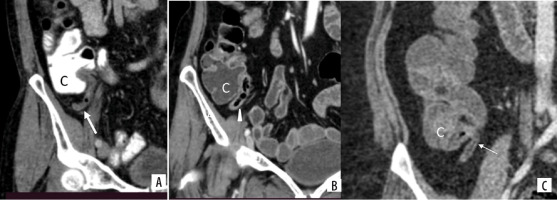
Figure 5
Contrast enhanced computed tomography images in axial plane show (A) and (B) post-ileal and pre-ileal locations of appendix (marked with arrow), with tip lying posterior and anterior to the distal ileum (IL), respectively. (C) Paracecal location with appendix lying lateral to the cecum (Ce)
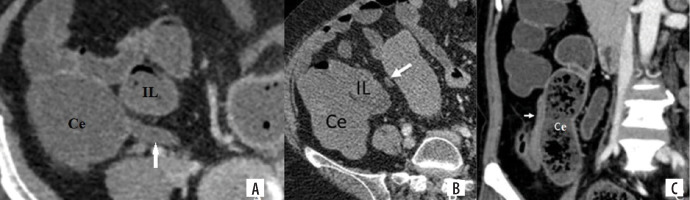
Figure 6
Contrast enhanced computed tomography images in coronal plane (A-D) show pelvic location of appendix (marked with arrow), with tip going down in the pelvic cavity
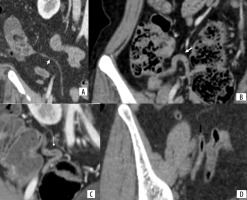
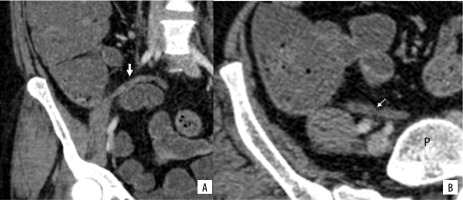
Figure 7
Contrast enhanced computed tomography images in coronal (A) and axial plane (B) show the appendix (marked with arrow) running upwards and medially to reach the front of sacral promontory (P)
Out of 400 patients with retrocecal appendix, 11 patients showed sub-hepatic location of appendiceal tip (Figures 3C and 3D, Table 1). The mean length of appendix was found to be 66.7 mm, ranging 6.3-123.0 mm. The appendiceal diameter varied 2.8-11.3 mm, with mean of 6.3 mm (Table 2). Wall diameter of less than 6 mm was noted in 817 (51.87%) patients, and with more than 6 mm was seen in 758 (48.12%) patients. The mean wall thickness was 2.37 mm, ranging 1.2-4.2 mm (Table 2). The majority of patients had wall thickness of less than 3 mm. Only 48 (~3%) and 2 patients (0.1%) had thickness of > 3, 4 mm each (Table 3). There was no statistically significant difference between gender and dia-meter (p = 0.183), or between age and diameter of normal appendix (p = 0.217). Similarly, no significant difference was observed between age and length (p = 0.192), gender and length of normal appendix (p = 0.224), age and wall thickness (p = 0.208), and gender and wall thickness of normal appendix (p = 0.118). In the present study, appendiceal lumen was filled with air only (in 177 of 1,575 patients, 11.2%), air mixed with hypo- or hyperdense material (in 1,111 of 1,575 cases, 70.5%), and only hypodense or hyperdense (in 287 of 1,575 patients, 18.2%) (Table 4).
Table 1
Distribution of different anatomical locations of appendix among study group
| Position | Number of patients | Percentage |
|---|---|---|
| Retrocecal | 400 | 25.3 |
| Sub-cecal | 320 | 20.3 |
| Post-ileal | 295 | 18.7 |
| Pelvic | 260 | 16.5 |
| Pre-ileal | 125 | 7.9 |
| Promontory | 125 | 7.9 |
| Paracecal | 50 | 3.1 |
Table 2
Measurement parameters of appendix among patients
| Parameter | Range (mm) | Mean (mm) | SD (mm) |
|---|---|---|---|
| Length | 6.3-123.0 | 66.7 | 21.3 |
| Diameter | 2.8-11.3 | 6.3 | 1.4 |
| Wall thickness | 1.2-4.2 | 2.4 | 0.4 |
Discussion
Appendix is an organ with wide variation in its position, length, diameter, and wall thickness. We often encounter a normal appendix with a diameter of more than 6 mm, and occasionally a normal appendix with a wall thickness of more than 3 mm can be seen. Conversely, we sometimes see patients with appendicitis without an increase in diameter, wall thickness, or peri-appendiceal inflammation, despite high clinical suspicion of appendicitis. There have been a number of studies evaluating the most common location of appendix with variable number of cases. In the present study, the most common location of the appendix was retrocecal (25.4%), followed by sub-cecal (20.3%), post-ileal (18.7%), pelvic (16.5%), and pre-ileal and promontory positions (7.9% each). The least common location in our study was paracecal. Our study correlated well with a study performed on cadavers that reported retrocecal (43.5%) as the most common position, followed by sub-cecal (24.4%), post-ileal (14.3%), pelvic (9.3%), and paracecal locations (5.8%), making pre-ileal (2.4%) as the least common position [9]. Wakeley [8] performed analysis of 10,000 cases, and found that the most common location was retrocecal (65.28%), followed by pelvic (31.01%), sub-cecal (2.26%), pre-ileal (1%), and post-ileal (0.4%) positions. The current study is not supporting the results of a study by Willekens [16], who reported that most common location is pelvic, followed by retrocolic or retrocecal, paracolic, and midline positions.
The diameter of appendix can vary widely, and depends on modality used to determine it. On ultrasound, the normal appendix appears as a compressible blind-ending tubular structure, with normal diameter of less than 6 mm from serosa-to-serosa [6]. The maximum diameter of normal appendix reported in the published literature ranges 6-10 mm [19]. In the present study, the diameter varied 2.8-11.3 mm, with a mean of 6.3 mm. Appendicular diameter greater than 6 mm was noted in about 48% of our patients, and in majority of these cases, the appendix was distended with air, fecal material, or contrast agent. Our findings are in accordance with a previous study by Benjaminov et al. [19], who reported mean diameter of appendix as 5.6 mm ± 1.3 mm (SD), ranging 3.0-11.0 mm, and more than 42% of the investigated population presented diameter above 6 mm. Our findings show that a dia-meter above 6 mm in the absence of other CT features of appendicitis is not a reliable cut-off value, as a considerably large proportion of our study subjects had a diameter up to 11.3 mm.
In the published literature, the maximum thickness of appendix was reported to be less than 2-3 mm [23]. Tamburrini et al. [17] reported that wall thickness of more than 3 mm may be considered a sign of inflammation. In the current study, the mean wall thickness was 2.37 mm, with the range 1.2- 4.2 mm. One important finding is that wall thickness of > 3 mm was noted in only 48 out of 1,575 patients (3%), and > 4 mm in only 2 out of 1,575 patients. Our findings correlated well with a previous study by Wille-kens et al. [16], who reported that mean wall thickness was 2.22 mm ± 0.56 mm, ranging 1.15-3.85 mm, with wall thickness of more than 3 mm seen in 8% of the subjects.
The length of appendix can influence symptoms and pathologies of the appendix. A very long appendix can reach up to sub-hepatic region and can mimic cholecystitis, hepatitis, or hepatic abscess. If it reaches deep down pelvic cavity, it can present as pathologies of pelvic organs. In our study, the length varied 6.3-123 mm, while the aver-age length was noted as 66.3 mm. While reviewing the lite-rature, we found that in only one study, appendiceal length was measured on CT [16]. The authors reported that the mean length of normal appendix was 81.11 mm ± 28.44 mm, with a range 7.2-158.8 mm. They also shown a correlation between appendiceal length and gender, but no correlation between appendiceal length and age or body length. They also suggested that the appendix is longer in children, and may become smaller after mid-adult life.
Our study has several advantages, the most important being large sample size and CT-based measurements of different parameters. However, it has few limitations, with the most important being lack of follow-up of patients included in the study. Secondly, we simply used patients’ history and clinical examination findings to create our inclusion criteria of non-appendicular signs and symptoms.
Conclusions
The appendix may exhibit a mystifying range of normal and abnormal appearances on CT. Knowledge of the location, appearance, and other characteristics of the normal appendix is important in accurately diagnosing cases of acute appendicitis. Although an appendix less than 6 mm may be considered normal, relying on appendix diameter alone may lead to misdiagnosis and mismanagement. One must be cautious while using size criteria alone since diameter above 6 mm has an overlap between a normal appendix and acute appendicitis. Therefore, it should be considered in association with clinical and secondary findings to avoid overdiagnosis and unnecessary appendicectomies. We strongly recommend that diameter-based CT criteria to diagnose appendicitis should be revised and standardized. Progressively more studies are warranted to obtain criteria for the same. Our study may become a reference to design larger studies in the future.






