Introduction
An internal hernia is defined as the protrusion of the abdominal viscera through a peritoneal or mesenteric aperture into a compartment in the abdominal and pelvic cavities [1,2]. It is reported to cause 0.6-5.8% of acute small bowel obstruction [3].
A sigmoid mesocolon-related internal hernia is a rare type of internal hernia that accounts for 6% of internal her-nias [2]. Historically, Benson and Killen [4] classified sigmoid mesocolon-related hernias into 3 subtypes: inter-sigmoid hernia, intramesosigmoid hernia, and trans-mesosigmoid hernia. Intersigmoid hernia was defined as the herniation of bowel loops into the intersigmoid fossa. The intersigmoid fossa is present in 50-80% of autopsies, with no difference between sexes [5]. It is an inverted V-shaped cul-de-sac situated at the top of the 2 roots of the parietal brim of the sigmoid mesocolon and is formed by a defect of fusion between the mesentery and the parietal peritoneum, so its space is enclosed by both structures [5]. The orifice points downward and slightly to the left [5,6]. Intersigmoid hernia has been reported as the most or the second most frequent type of sigmoid mesocolon-related internal hernia [4,7]. Intersigmoid hernia is treated with surgery, but preoperative diagnosis is difficult because of the few of specific clinical and radiological findings [7,8]. Computed tomography (CT) is an important diagnostic tool for internal hernias [9], but the CT findings of intersigmoid hernia has been little reported, and most of them were single case reports or review articles [7,10]. Thus, we evaluated the CT findings of 7 patients who were surgically diagnosed with intersigmoid hernia.
Material and methods
Patient population
After obtaining institutional review board approval from all 3 institutions, we searched for patients suspected of having intersigmoid hernia from their radiology reporting databases between April 2010 and March 2018. Nine patients were initially included. Two were excluded because of a lack of surgical confirmation of diagnosis. Finally, 3, 2, and 2 cases were enrolled from 3 institutions, respectively, for a total of 7 cases.
Computed tomography technique
All CT examinations were performed with a 4-, 32-, and 64-row CT scanner (Asteion 4; Toshiba Medical Systems, Aquillion 64; Toshiba Medical Systems, Light Speed VCT; GE, light speed 32; GE). One patient underwent only an unenhanced CT scan. Others underwent both unenhanced and enhanced CT scans, either single-phase (n = 2) or biphasic (n = 4). About 100 ml of nonionic intravenous contrast medium (iohexol [300 mgI/ml], iopamidol [300 mgI/ml], iopamidol [370 mgI/ml]) were administered at a rate of 3 ml/sec (biphasic) or 2 ml/sec (single-phase). Biphasic CT scans were performed at 40- and 80-sec delay (n = 2) or 40- and 110-sec delay (n = 3). Two patients underwent a single-phase CT scan with 180-sec delay. All cases were reconstructed in the axial and coronal planes. The slice thickness was 1-7 mm in the axial plane and 3-5 mm in the coronal plane. Detailed image acquisition protocols are listed in Table 1.
Table 1
Image acquisition protocol
Image analysis
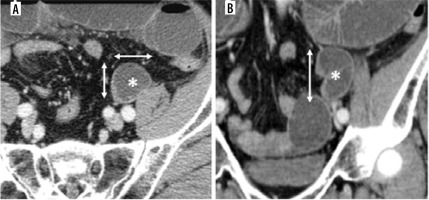
Two radiologists with 6 and 21 years of experience in abdominal radiology, who were blinded to the clinical data and diagnosis, independently reviewed all CT images to measure the intersigmoid fossa and evaluate the anatomic relationship between the bowel loop and adjacent organs, including superior sigmoid vessels, sigmoid vessels, sigmoid colon, left psoas muscle, left gonadal vein, and left ureter. If there was disagreement between the 2 opi-nions, we discussed and integrated the opinions. To estimate the size of the intersigmoid fossa, we measured the size of the strangulated small bowel loop in the lateral and anterior-posterior length at the largest section of the axial plane and the caudal-cranial length at the largest section of the coronal plane (Figure 1). For estimation of the location of the orifice of the intersigmoid fossa, the vertical distance between the bowel occlusion point and bifurcation of the left common iliac artery in the coronal plane was also measured (Figure 2). If the occlusion point and bifurcation were not present in the same coronal plane, we first identified the caudal-cranial level of the bifurcation point in the horizontal section and then measured the linear distance from the occlusion point to the level of the bifurcation on the coronal section. We estimated the volume of the intersigmoid fossa using the formula for the volume of an ellipse volume (V= lateral length × anterior-posterior length × caudal-cranial length × 3.14 × 1/6). To compare with Somé’s report [5], we also calculate the volume of the intersigmoid fossa using the formula of a truncated cone volume (V = lateral length × anterior-posterior length × caudal-cranial length × 1/3).
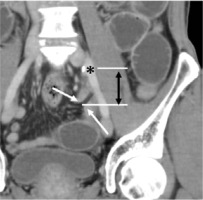
Figure 1
61-year-old man with intersigmoid hernia. A) Axial and (B) coronal contrast-enhanced computed tomography images show the small bowel loop in the left side of the pelvic space (asterisk). We measured the size of the loop in the lateral and anterior-posterior length at the axial plane and the caudal-cranial length at the coronal plane in each largest section (2-headed arrow)
Results
All cases were male, the mean age (standard deviation, range) was 61.0 (13.1, 36-85) years, the mean height was 166.9 (2.2, 165.0-170.0), the mean body weight was 54.9 (7.0, 44.4-65.0), and the mean BMI was 19.7 (2.6, 17.0-23.7). All cases presented abdominal pain and nausea. The average time from onset to CT imaging was 1.3 days, and the average time to surgery was 5.1 days. One case had a history of laparoscopic resection for colon cancer, but there was no other history of abdominal surgery. Intraoperative findings showed no intestinal necrosis in all cases, and the patient was treated with release of the incarcerated bowel. Detailed patient characteristics are listed in Table 2.
Table 2
Patient characteristics
The mean size of the bowel loops (standard deviation, range) was 5.2 (1.3, 4.0-8.3) cm in the caudal direction, 3.6 (0.8, 2.5-5.1) cm in the lateral, and 3.4 (0.6, 2.5-4.7) cm in the anterior-posterior direction. The mean volume of the intersigmoid fossa calculated using the formula for the volume of an ellipse volume was 37.9 (27.8, 18.3-103.0) cm3. The mean volume of the intersigmoid fossa calculated by using the formula of a truncated cone was 24.0 (17.7, 9.9-65.6) cm3. The point of obstruction of the small bowel was located inferior to the bifurcation of the left common iliac artery and was 3.6 (0.6, 2.8-4.7) cm caudal (Table 3).
Table 3
Size of small bowel loop and vertical distance between bowel occlusion point and bifurcation of left common iliac artery
* Volume of intersigmoid fossa estimated by using the formula for the volume of an ellipse (V = lateral length × anterior-posterior length × caudal-cranial length × 3.14 × 1/6).
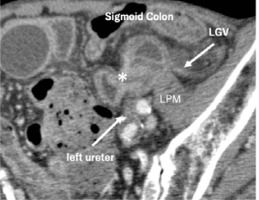
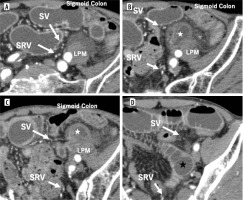
In all cases, the small bowel ran under the point that the inferior mesenteric vessels bifurcated to the superior rectal vessels and the sigmoid vessels. It formed a sac-like appearance between the left psoas muscle and the sigmoid colon (Figure 3). In addition, the ureter ran dorsal to the point of the bowel stenosis, and the left gonadal vein ran outside the small bowel loops (Figure 4).
Figure 3
85-year-old man with intersigmoid hernia. A-D) Contrast-enhanced computed tomography images in arterial phase from cranial to caudal section. B, C) Small bowel loop (white star) lies between the sigmoid colon and the left psoas muscle (LPM). D) The dilated bowel (black star) runs under the point at which the inferior mesenteric vessels bifurcated to the superior rectal vessels (SRV) and the sigmoid vessels (SV)
Discussion
Intersigmoid hernia is the herniation of the small bowel into the intersigmoid fossa [4]. CT plays an important role in the diagnosis of internal hernias, including intersigmoid hernias. The diagnosis of internal hernia with CT images consists of identifying the sac-like appearance of the strangulated small intestine and the causative congenital structures on the surrounding vasculature and organs [10-13]. A sac-like appearance is a direct sign of an internal hernia. This means a fluid-filled, distended intestinal loop or a radial array of distended loops with stretched and thickened mesenteric vessels converging to a central point [10,13]. The CT findings of intersigmoid hernia have already been reported as an entrapped small bowel that shows a sac-like appearance between the stretched sigmoid colon and the left psoas muscle [7,8]. However, to the best of our knowledge, no studies have investigated the CT findings in multiple intersigmoid hernia cases.
In this study, we evaluated the CT findings of seven intersigmoid hernia cases and found the following findings in all cases: The small bowel (a) ran under the point at which the inferior mesenteric vessels bifurcated to the superior rectal vessels and the sigmoid vessels (Figure 3 and 5A), (b) was strangulated at the anterior of the left ureter (Figure 4 and 5B), (c) formed a sac-like appearance (d) medial to the gonadal vein (Figure 4 and 5B), and (e) lay between the left psoas muscle and the sigmoid colon (Figure 4 and 5B). Among these findings, (c) and (e) are consistent with previous reports. Because the intersigmoid hernia is the only internal hernia that related to the intersigmoid fossa, the remaining findings (a, b, d) will be discussed based on the anatomy of the intersigmoid fossa.
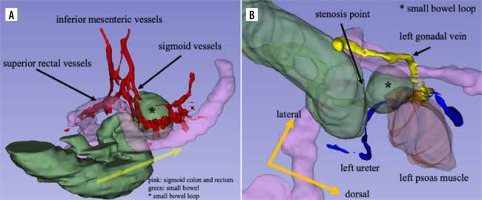
Figure 5
62-year-old man with intersigmoid hernia. A) Volume rendering (VR) images were created by segmenting each organ in the contrast-enhanced computed tomography images using a 3D-slicer, which is a free, open-source software application for the visualization and analysis of medical image computing datasets. A Front view of the VR image shows the small bowel running under the point that the inferior mesenteric vessels bifurcated to the superior rectal vessels and the sigmoid vessels (yellow arrow). B) Caudal view of the VR image shows the left ureter running dorsally to the stenosis point. The left gonadal vein runs laterally at the small bowel loop (*)
Some structures surround the orifice of the intersigmoid fossa; dorsal to the orifice is either the left common iliac artery or 2 branches of bifurcation (left internal or external iliac artery) and ureter, and above it is the superior rectal artery and the sigmoid arteries [6]. Somé et al. reported in their cadaver study that the most frequently encountered structures during the dissection of the intersigmoid fossa fundus were the ureter, the common iliac artery, the gonadal pedicle, and the left external iliac artery [5].
As for the finding in (a) and (b) above, it is consistent with the description that the ureter was situated dorsal to the orifice and the superior rectal artery and the sigmoid arteries above [6]. As for (d), there is a description of the gonadal pedicle running backward to the intersigmoid fossa fundus [5], but we could not find any report of it running laterally to the intersigmoid fossa.
Despite no sex differentiation in the presence of intersigmoid fossa [5], all patients were male. In females, the uterus may inhibit the protrusion of the small bowel into the intersigmoid fossa because of its position. The intersigmoid fossa is located near the ovarian fossa, which is surrounded posteriorly by the ureter and the internal iliac artery, and superiorly by the external iliac artery [14]. Therefore, the left ovary may prevent small bowel protrusion. These anatomical features may explain the sex differentiation of the presence of intersigmoid hernia in this study.
We evaluated the size of the intersigmoid fossa by measuring the diameter of the small bowel loop. In all cases, the diameter in the craniocaudal direction was the longest, and the diameters in the lateral and anterior-posterior directions were comparable. Chiarini et al. [8] and Somé et al. [5] reported the size of intersigmoid fossa in previous studies. Chiarini et al. reviewed 114 studies of intersigmoid hernia including 122 cases treated by surgery and reported that the mean size of intersigmoid fossa in 96 patients with intersigmoid hernia was 2.65 cm (SD 1.15 cm, range 1-10 cm). Somé et al. measured the size of orifice (transverse and longitudinal diameter, TD, and LD) and depth of fossa in 48 cases of cadavers and calculated the volume by applying the formula of the truncated cone volume (volume = TD × LD × depth × 1/3). They reported that 55.5% of cases were smaller than 4 cm3, and 13.9% were larger than 9 cm3. Our results tended to be larger than the findings of Chiarini et al. and Somé et al. Differences in the measurement and calculation methods may explain the differences between our results and those of previous reports. It may also be a factor that the herniated bowel stretches the intersigmoid fossa, increasing its size in this study.
Regarding the orifice location, Testut described that the left common iliac artery is situated dorsal to the orifice [6], whereas in all our cases the orifice was located inferior to the bifurcation of the common iliac artery. This difference can be explained by the difference between a cadaver and a living body, and the fact that our study is only an estimation based on CT findings. It is also possible that our cases may have a lower orifice position, and the lower position of the orifice may correlate with the risk of intersigmoid hernia.
Our study had several limitations. Although reconstructed images in 2 or more directions were obtained in all cases, the image acquisition protocol was inconsistent. This variety may not be a significant problem in assessing anatomical evaluation but may cause some bias. Although there have been reported cases requiring resection of the small bowel due to ischaemia [8], all our cases were treated by the reduction of the incarcerated hernia. This bias may be due to the small sample size. Further investigations with a larger sample size are required.
Conclusions
All cases showed common imaging findings, which were considered possible characteristic findings.
The estimated position of the fossa was lower, and the size of the fossa was larger than in the previous study. This difference may be attributed to differences in measurement methods, but the large size and the lower position of the fossa was considered a possible risk factor.