Introduction
Percutaneous drainage is a standard method of management of abdominal and pelvic fluid collections and should be considered the treatment of choice because it is associated with lower morbidity and mortality than surgical drainage [1]. According to the standards of practice published by the Society of Interventional Radiology [2], percutaneous drainage should be performed when fluid collection could be infected, when the fluid sample needs to be collected for characterisation, when the collection is causing symptoms, or when the procedure is necessary for another intervention to be possible. Percutaneous drainage can be used to avoid surgery or to improve its results (e.g. in Crohn’s disease and diverticular abscess).
The drain can be placed in the abscess with one of two techniques. When the trocar technique is used, the cathe-ter is mounted on a sharp trocar, and both are inserted together in a single step. Some interventional radiologists use the tandem trocar technique, which requires 2 punctures. First the collection is punctured with a needle and aspirated, and then the catheter is inserted parallel to the needle. On the other hand, there is the Seldinger technique, which involves the insertion of a guidewire into the fluid collection and subsequent placement of the drain over the wire. The trocar technique is easier and faster than the Seldinger technique even when the tandem trocar technique is used [3,4].
The most commonly used drain diameters range from 6F to 14F; however, the effectiveness of small-bore drains has not been clearly established. The aim of this study was to evaluate whether small-bore drains can be used in purulent collection drainage as well as to determine whether there are any features predictive of clinical failure of percutaneous drainage.
Material and methods
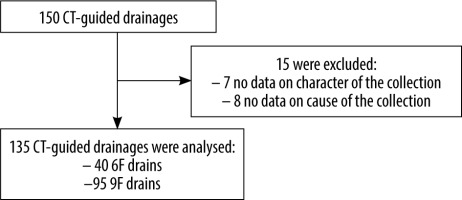
The search of the prospectively maintained database of computed tomography (CT)-guided drainages of abdominal or pelvic fluid collections was performed. It returned 150 procedures performed in consecutive patients from a single centre. However, 15 cases were excluded from the analysis due to the lack of data on character or cause of the collection (Figure 1). All procedures were performed under CT-guidance (Aquilion One, Toshiba, Japan). An unenhanced CT scan was done at the beginning of the procedure to visualise the size and location of the fluid collection and to plan a suitable path for the drain. Local anaesthesia (2% lidocaine) was used in all procedures. The one-step trocar drainages were performed with 6F or 9F drains (Balton, Poland). An unenhanced CT scan was done after the procedure to evaluate the location of the drain and assess possible complications. The drain was attached to the skin with non-absorbable sutures and was removed when daily output was < 20 ml of fluid.
Operators made the choice between 6F or 9F cathe-ters. 6F catheters were usually preferred in small collections (< 5 cm in diameter), when thin fluid was expected, and in patients with a high risk of bleeding (INR > 1.4, proximity to arteries, long intrahepatic trocar pass). Patients with a platelet count below 50,000/μl and an INR of 1.5 or greater were excluded due to excessive risk of bleeding.
The interventions were done by 3 interventional radio-logists with at least 8 years of experience in CT-guided drainage. The following parameters were collected: patients’ age and sex, drain size, radiation dose (dose length product [DLP]), as well as mean diameter, location, and content of the fluid collections.
Technical success was defined as insertion of the drain into the fluid collection and aspiration of the fluid sample. Clinical success was defined as complete resolution of the infection requiring no further surgical intervention [2] or placement of a larger drain. Multiple drainages with small-bore drains were also classified as successful if no surgery or insertion of a higher-bore drain (upsizing) was necessary.
Complication rates were assessed and classified according to the Clavien-Dindo [5], Society of Interventional Radiology [6], and Cardiovascular and Interventional Radiological Society of Europe classifications [7].
The Bioethical Committee waived the requirement for written consent due to the retrospective nature of this study. All procedures were performed in accordance with the declaration of Helsinki of 1964. Informed consent for the procedure was obtained from all the patients.
Statistical analysis
Fisher’s exact test was used to evaluate for significant diffe-rences in categorical variables whereas the Mann-Whitney U test was performed to assess quantitive variables. The p-value of < 0.05 was considered significant. Statistical analyses were performed using the R software package (http://www.r-project.org/).
Results
The analysed cohort consisted of 135 patients (91 males and 44 females) aged 60.5 ± 14.5 years (20-90 years). Procedures were done using the one-step trocar technique with 6F catheters for 40 procedures and with 9F catheters for 95 procedures. The mean size of the abscesses was 77.0 ± 28.8 mm (32-220 mm).
Most common collections were intrahepatic and located in the peripancreatic region (Table 1). The collections were related to various causes, most commonly due to postoperative complications (n = 75), acute pancreatitis (n = 24), or biliary origin (n = 20); less common causes included other intraabdominal inflammatory processes (n = 14), ruptured aortic aneurysm (n = 1), or ruptured tumour (n = 1).
Table 1
Location of the collections
| Location | n (%) |
|---|---|
| Peripancreatic | 36 (26.7) |
| Other retroperitoneal | 6 (4.4) |
| Intrahepatic | 43 (31.9) |
| Perihepatic | 13 (9.6) |
| Subphrenic | 10 (7.4) |
| Other intraperitoneal | 21 (15.6) |
| Pelvic | 6 (4.4) |
Thick fluid collection was found in the majority of collections; thin fluid was aspirated only in a few cases (Table 2).
Technical success was achieved in 100% of cases. Five (3.7%) patients required surgical drainage because the percutaneous method did not give satisfying results. Two (1.5%) patients required upsizing of the drain (from 9F to 12-14F) (Table 3). Clinical success, defined as resolution of infection without surgery or upsizing of the drain, was achieved in 128 (94.8%) patients.
Table 3
Characteristics of the patients with drainage failure
Ten patients underwent 2 drainages (6 postoperative, 3 acute pancreatitis, 1 biliary origin), and 3 patients had 3 drainages (2 postoperative and 1 acute pancreatitis). In 8 cases, repeated drainage was needed because the drain was accidentally removed by the patient or a nurse. In 4 patients, repeated drainage was needed because the abscess recurred after drain removal. In 2 patients, the second drain was needed as the output was too low.
Of these 13 patients, 2 required large-bore drains (12F or 14F) after failure with 9F drains. The Seldinger technique was used with larger (12F and 14F) drains (Cook, Bloomington, IN, USA). Insertion of large drains was successful both technically and clinically in these 2 patients.
The mean radiation dose in terms of DLP was 617 ± 467 mGy × cm (160-3799 mGy × cm). The mean procedure time was 28.0 min ± 11.3 min (9-84 min).
Three (2.2%) patients presented with Clavien-Dindo grade III complications: one pneumothorax (managed with drainage), one case of peritonitis (managed with surgery), and one case of bleeding (managed with embolisation). The bleeding occurred 2 weeks after the procedure; prolonged friction of the catheter against a branch of the gastroduodenal artery was the suspected cause. The 3 complications were also of grade III according to the Society of Interventional Radiology and Cardiovascular and Interventional Radiological Society of Europe classifications [6,7]. None of the patients presented with higher-grade complications (Table 4).
Table 4
Periprocedural complications
| Type of complication | Number | ||
|---|---|---|---|
| Clavien-Dindo grade III | 3 | (2.2%) | |
| Pneumothorax (managed with drainage) | 1 | ||
| Peritonitis | 1 | ||
| Delayed bleeding (managed with embolization) | 1 | ||
In statistical analysis the study group was divided based on the size of the drain. Statistical analysis to compare efficacy of the drainage between the 6F and 9F subgroups was performed; however, the size of the collections differed significantly (p = 0.004) between the subgroups. Therefore, both subgroups were matched 1 : 1 based on the mean size of the collections to avoid bias. Statistical analysis using Fisher’s exact test showed no significant difference in clinical success rate between the 6F and 9F subgroups in both cases of collection size-matched and nonmatched subgroups (Table 5).
Table 5
Clinical success rate between 6F and 9F subgroups
| 6F | 9F | p-value | |
|---|---|---|---|
| Clinical success in nonmatched subgroups | 40/40 (100%) | 88/95 (92.6%) | 0.104 |
| Clinical success in matched subgroups | 40/40 (100%) | 37/40 (92.5%) | 0.240 |
Furthermore we analysed the study population based on the clinical success or failure of the drainage looking for significant predictive variables of clinical failure of the drainage (Table 6). The only feature that reached a level of statistical significance was the mean size of the collection (p = 0.038).
Table 6
Variables predictive of drainage clinical success
Discussion
CT-guided percutaneous drainage is a standard procedure to manage abdominal and pelvic abscesses. How-ever, there are few articles available on the use of small-size drains, especially for collections with thick content. This study showed that using very small and small drains (6F and 9F) can give very good technical (100%) and clinical (94.8%) results with a low rate of major complications (2.2%). It is worth noting that the majority of the cohort (95.5%) had thick fluid collections. Statistical analysis showed that there is no difference in clinical success rate between 6F and 9F. Moreover, the size of the collection was the only predictive feature associated with increased risk of failure of the percutaneous drainage.
In the study by Rotman et al. [8], the patients did not benefit from using larger-bore drains (> 10F). However, as the authors reported, small-bore drains (< 10F) were used only for thin collections. The results of this study show that small-bore drains (6F and 9F) are adequate for intraabdominal abscesses with both thick and thin content.
Röthlin et al. [9] reported no significant difference between 7F and 14F catheters inserted under ultrasound guidance in terms of success rate (83% and 85%, respectively). However, the study was done more than 20 years ago, and reported success rates are higher in more recent studies. Our findings are in agreement with the publication by Röthlin et al. suggesting that small-bore drains (7F) are effective for abscess drainage. The higher success rates seen in our study are probably related to the use of CT guidance rather than ultrasound guidance.
The randomised study by Gobien et al. [10] in 1985 reported low efficacy of 6F drains due to clogging and no significant difference in efficacy between 8F and 12-14F drains. However, the 6F drains were used in only 5 patients, and this group was not included in the statistical analysis.
In the study by Kajiwara et al. [3], an 18G needle was inserted into an abscess and its position was confirmed by content aspiration. A catheter with a trocar was then inserted next to the 18G needle to drain the abscess. In our opinion, the double puncture is not necessary, and abscesses can be drained with a catheter only. CT guidance provides excellent spatial resolution and allows the needle to be placed with great accuracy. The study by Kajiwara et al. [3] reported a similar clinical success rate (93.5%) to that seen in our study.
The radiation dose in terms of DLP, the duration of the procedure, and mean abscess size were similar to those reported in other publications [3,11-14].
Very few Clavien-Dindo grade III complications occurred in the studied group (2.2%). This is in line with complication rates in previous publications [11] and the Society of Interventional Radiology guidelines [2], which suggest a 2.0-8.0% major complication rate threshold.
The results of this study suggest that small-bore drains can be used in abdominal or pelvic abscesses as a first-line treatment method. No tandem-trocar technique is necessary. Larger-bore drains are usually inserted using the Seldinger technique, which is more complicated and takes more time. Additionally, CT-fluoroscopy (one-step/quick-check method) does not always allow visualisation of the whole guidewire, as opposed to small-bore drains inserted with the trocar technique.
The limitations of this study include its retrospective design, as well as the fact that the study group consists of patients from a single institution. The drains (6F and 9F) were not chosen randomly by the radiologists, and this could lead to bias, which we tried to reduce by matching size of the collections in the 6F and 9F subgroups.
Conclusions
The results of this study show that percutaneous CT-guided abscess drainage with small-bore drains is usually sufficient to obtain clinical success with a low complication rate. The size of the collection is the only feature in our study that is associated with increased risk of failure of the percutaneous drainage. Further studies are needed to determine potential cut-off values above which insertion of a large-bore drain or multiple drains should be considered. Insertion of a large-bore drain or surgery can be considered in rare cases of failure of drainage with a small-bore drain.