Introduction
Pelvic pain, either related or unrelated to menstruation, is especially common in women of reproductive age. If this pain lasts longer than 6 months, it is called chronic pelvic pain (CPP) [1]. This pain may have gynaecological causes, such as endometriosis, adenomyosis, uterine myoma, ovarian cysts, and pelvic venous congestion syndrome (PVCS), or occur as a result of urological, gastrointestinal, and even psychological factors. Thirty-nine per cent of all women suffer from CPP at some point in their lives [1,2], and PVCS is the reason for this pain in 30% of cases [3]. The association between CPP and pelvic varices was first described by Richet in the 19th century [4]. Since then, many different definitions have been made. However, today, it is defined as pelvic and perineal fullness due to reflux secondary to insufficiency or obstruction in the ovarian and/or pelvic veins, pain during and after sexual intercourse, the need to urinate, and accompanying perineal, vulvar, and lower extremity varices [5].
Although radical treatments, such as total hysterectomy and bilateral oophorectomy have been tried in the treatment of PVCS, ovarian vein ligation is applied as the most common surgical treatment method [6]. Endo-vascular ovarian vein embolization, which was first described in 1993, is currently the primary treatment method, considering the shorter hospital stay, fewer and milder complications compared to surgical treatments, and reproducibility of treatment [7].
This study aimed to determine factors affecting the success of endovascular venous embolization used in the treatment of PVCS and present long-term treatment results.
Material and methods
In this study, the data of 144 female patients who underwent endovascular ovarian vein embolization due to PVCS between January 2012 and July 2020 were retrospectively analysed. The study was evaluated and approved by the local Ethics Committee.
The primary objective of the study was to determine the efficacy of treatment, and the secondary objective was to determine whether treatment efficacy was related to parity, the embolizing agent used, pre- and post-menopausal status, and the number of veins with pre-procedure insufficiency.
Patient population
The population of this study consisted of patients who presented to gynaecology and cardiovascular surgery outpatient clinics due to pelvic varicose veins and were referred to us for diagnosis and treatment. Of the 144 patients, 93 (70.4%) were in the reproductive period and 39 (29.5%) were in the post-menopausal period, with a mean age of 44 (min: 26, max: 72) years. Demographic and clinical data are shown in Table 1. The following inclusion criteria were used: 1) having at least a six-month history of CPP, 2) undergoing a contrast-enhanced computed tomography (CT) examination before the procedure, and 3) attending the postoperative clinical follow-up for at least 3 months. The exclusion criteria were as follows: 1) absence of CT imaging for diagnosis before treatment, 2) being younger than 18 years, and 3) presence of any secondary pathology that could cause venous congestion.
Table 1
Demographic features and clinic findings
Diagnosis
The patients were first evaluated with transabdominal pelvic venous Doppler ultrasonography (US). In the US examination, patients with non-saphenous varicose veins and CPC were considered suspicious for PVCS. Then, those suspected to have PVCS underwent contrast enhanced biphasic abdominal CT imaging, including the arterial phase obtained at 15 seconds and the venous phase obtained at 70 seconds. The patients with enlarged (> 6 mm) pelvic venous structures and/or significant reflux were diagnosed with PVCS, and the decision to operate was taken. In addition, the presence of contrast in the ovarian vein in the late arterial phase and the presence of a pelvic varicose vein were considered to be supporting signs accompanying ovarian vein dilatation for diagnosis. For the patients who did not have typical radiological findings but presented with symptoms consistent with clinical PVCS, diagnostic angiography was performed for a dynamic venous examination, and embolization was applied to these patients if dilatation and/or reflux was detected.
Treatment
The procedures were performed by 2 interventional radiologists with more than 10 years of experience in interventional radiology. After local anaesthesia of the inguinal region, the right main femoral vein was punctured under US guidance. A 6-Fr introducer was placed, and then the left and right renal veins were selectively catheterized one by one using 5-Fr cobra (Terumo, Europe) and 5-Fr simmons1 (Cordis Johnson & Johnson, Europe NV, Roden, Netherlands) macrocatheters advanced over a 0.035 hydrophilic wire (Glidewire, Terumo Europe). Venographs were obtained under the Valsalva manoeuvre. The ovarian vein on the side with signs of venous insufficiency was embolized with a 2.7-Fr (Renegade, Boston Scientific, USA) microcatheter and superselectively catheterized with a metallic coil, vascular plug, and 1-3% aethoxysklerol transformed into foam (Figure 1). Embolization was achieved with the use of a coil alone in 47 patients (32.6%), while other materials were additionally used in 97 (67.3%) patients. The embolizing material to be used was determined according to the diameter width of the venous structure. A vascular plug was used for veins with a diameter of 10 mm and larger. For venous structures thinner than 10 mm, embolization was performed with a coil. Aethoxysklerol was used in the first patients who underwent treatment, but it was not used again in subsequent treatments because it caused temporary abdominal pain in patients. Procedural data are shown in Table 2. The patients who did not develop any complication after the procedure were discharged from the hospital on the same day with recommendations.
Figure 1
A 39-year-old female patient was admitted to our hospital due to pelvic pain lasting for one year. The examination revealed bilateral pelvic venous insufficiency on ultrasound and computed tomography. The patient was admitted to the angiography unit for therapeutic purposes. The left and right ovarian veins were catheterized with transfemoral approach, respectively. In the venograms performed under the Valsalva manoeuvre, insufficiency of both ovarian veins, and parauterine and paraovarian varicose veins were detected (A, B). Subsequently, the bilateral ovarian veins were embolized with a coil (C). The procedure is terminated
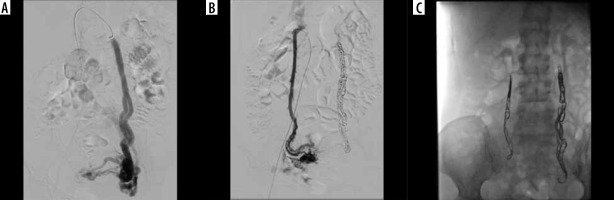
Table 2
Procedural data
The pain levels of the patients before and after the procedure were graded using the Visual Analogue Scale (VAS). For this evaluation, a scale consisting of 9 items, as recommended by the Society of Interventional Radiology, was administered to assess pelvic and lower extremity pain felt while lying down and standing up, dyspareunia, the relationship between pelvic pain and menstruation, urinary urgency, and use of analgesia [8]. The patients evaluated pain by scoring each item from 1 to 10. The efficacy of treatment was evaluated using the VAS at baseline and at the 3rd , 6th, and 12th months after the procedure. By comparing the pre- and post-procedure pain scores, 80-100% reduction in pain was considered as ‘very successful’, 50-80% reduction as ‘successful’, and <50% reduction as ‘unsuccessful’ pain management.
Statistical analysis
TURCOSA (Turcosa Analitik Ltd., Turkey) statistical software was used for the statistical analysis of the data. In the presentation of descriptive data, percentage and number values were obtained for categorical variables, and mean and standard deviation (SD) values were obtained for noncategorical continuous variables. The χ2 and Fisher’s exact χ2 tests were used to compare qualitative data. Quantitative data were tested for normality of distribution and homogeneity before comparisons, and quantitative data with a normal distribution were compared using Student’s t-test. For statistical tests, a p-value below 0.05 was considered statistically significant.
Results
Pelvic CT performed before the procedure revealed unilateral insufficiency in 75 (52.08%) patients and bilateral insufficiency in 69 (47.9%). Unilateral insufficiency was usually on the left side, with insufficiency findings being observed in the left ovarian vein in 59 (40.9%) patients and the right ovarian vein in 16 (11.1%). Venography performed before embolization showed unilateral insufficiency in 73 (50.7%) patients and bilateral insufficiency in 71 (49.3%), and embolization was performed accordingly. In 2 patients, angiography was performed due to the presence of symptoms, although radiological findings were not present on CT. Embolization therapy was performed due to the detection of insufficiency on angiography.
There were 144 patients attending the third-month follow-up, 99 patients attending the sixth month follow-up, and 84 patients attending the 12th-month follow-up.
Complete vascular occlusion was achieved in all the procedures, and the rate of technical success was 100%. According to the evaluation of treatment efficacy according to the reduction in pain scores at the third-month follow-up, pain management was very successful in 37 (25.6%) of the 144 patients, successful in 55 (38.1%), and unsuccessful in 52 (35.3%). The mean pain score was 35.4 (min: 2, max: 82, SD: 15.9) before the procedure, 14.6 (min: 0, max: 47, SD: 11.7) at the 3-month follow-up, 12.2 (min: 0, max: 64, SD: 11.3) at the 6-month follow-up, and 14.1 (min: 0, max: 67, SD: 13.6) at the 12-month follow-up. Changes in VAS scores during follow-up are shown in Table 3 and Figure 2.
Table 3
Changes in VAS scores during the follow-up
| Factor | n | Mean ± SD (Min.–Max.) |
|---|---|---|
| Preoperative | 144 | 35.46 ± 15.9 (2-82) |
| Postoperative 3rd month | 131 | 14.68 ± 11.7 (0-47) |
| Postoperative 6th month | 99 | 12.27 ± 11.3 (0-64) |
| Postoperative 12th month | 84 | 14.14 ± 13.6 (0-67) |
Treatments applied using a coil alone were significantly more successful in pain management than those involving the use of different additional materials in addition to the coil (p = 0.036) (Figure 3). Furthermore, the patients with unilateral insufficiency before the procedure were found to have more successful pain management than those with bilateral insufficiency (p = 0.041) (Figure 4). Lastly, reproductive/postmenopausal status and parity had no statistically significant effect on treatment efficacy (p = 0.250 and p = 0.573, respectively).
Discussion
CPP and PVCS are common health problems in women. With emerging medical technologies, many alternative treatment methods have been developed. Although percutaneous pelvic venous embolization is currently the most commonly used treatment method, there is no evidence of its success provided by comparative clinical studies with a control group. Nevertheless, endovascular embolization is recommended for treatment by the Society for Vascular Surgery and the American Venous Forum in the presence of 2B-grade evidence [9].
Although endovascular embolization has superior features, such as increased patient comfort and shorter hospital stay, it also has certain negative aspects, including radiation applied to the pelvic region and the high cost of many embolizing materials used to provide complete closure, especially in women of reproductive age.
In the current study, in which we retrospectively evaluated 144 patients who underwent pelvic venous embolization, we obtained successful results in 64.6% of the patients. The results are consistent with the success rates reported in the literature, varying between 30 and 90% [10-13].
The most controversial issue in the efficacy of treatment is the choice of which vessels to embolize. While some studies in the literature suggest that only left ovarian vein embolization may be sufficient [9], there are also authors arguing that both ovarian veins should be closed [10]. Some authors act more radically and argue that both pudendal veins and both ovarian veins should be closed [11,14,15]. In the current study, only the ovarian veins with reflux and dilatation were embolized, and the healthy veins were preserved. This was to reduce the procedure time and the radiation dose taken by the patient, as well as to decrease the cost of materials.
In this study, we observed that postoperative pain management in patients with bilateral venous insufficiency was more unsuccessful than in those with unilateral insufficiency. This was attributed to the collaterals and pathological drainage becoming more complicated as the number of vascular beds remaining in a congested state increased in the pelvic venous system [16]. For example, undiagnosed isolated iliac vein insufficiency may have affected this condition. Therefore, it may be important to evaluate the iliac veins on angiography during treatment. In addition, the increase in the number of embolizing materials used may increase the level of inflammation, and thus complicate pain management [17].
As another significant finding, pain management was found to be more effective in procedures performed using only coils. This was considered to be because the inflammatory property of sclerosant materials used was higher than that of other mechanical embolizing materials. In contrast, a previous study comparing coils and other embolizing materials reported no significant difference in pain management [13].
We determined that parity and menopause had no effect on pain management. It is known that parity and blood pooling due to increased venous capacity during pregnancy are involved in the aetiology of pelvic pain during and after pregnancy [18-21]. The literature contains no study showing the effect of previous pregnancies on treatment success. However, it is considered that pregnancy after treatment may lead to recurrence in terms of PVCS. In a study conducted with 12 infertile patients who successfully conceived after pelvic venous embolization, pregnancy and PVCS were reported to be in an absolute relationship [22].
The retrospective nature of the study and the short-term follow-up of the patients can be considered as limitations. In addition, as in all publications in the lite-rature using VAS scoring, the pain level of the patients was subjectively evaluated. The results of VAS may vary depending on the different pain thresholds of patients or the presence of accompanying chronic diseases (another pathology that can increase the use of painkillers, such as migraine accompanying PVCS). As a result, the evaluation of response to treatment is not objective in every patient. Lastly, the results of the study were not highly conclusive due to the absence of a control group and the non-homogeneous distribution of the data or sample.
Conclusions
Endovascular pelvic venous embolization is an important option in the treatment of PVCS due to its less invasive and reproducible nature. More satisfactory results can be obtained by revealing variables affecting the success of treatment in further prospective studies that will include a control group and evaluate the results over a longer follow-up.