Introduction
Primary hyperparathyroidism is a common endocrine disorder caused by parathyroid adenomas, hyperplasia of the parathyroid glands, or carcinomas in rare cases. The only curative treatment is complete surgical resection of these lesions [1,2].
During surgery, it is extremely important for curative treatment to appropriate identification of tumours of the thyroid and parathyroid glands, and also to reduce the need for surgical exploration of the neck [3].
It can be difficult to locate abnormal parathyroid glands accurately, efficiently, and safely. For diagnosis and surgical planning, preoperative imaging can be performed using different imaging modalities. Currently available imaging modalities consist of ultrasound (US), radionuclide scanning, magnetic resonance imaging, and computed tomography (CT), often used in combination [1,2].
US provides the surgeon with direct, dynamic information about the target tumour location in relation to other anatomical landmarks that can be identified as coordinates. Even in US performed as preoperative preparation, the localisation of some tumours may be confusing [4,5].
Furthermore, the first reported use of intravenous administration of high doses of methylene blue (MB) was in 1971 by Dudley et al., to identify intraoperative parathyroid adenomas. However, administration of high doses of MB (7.5 mg/kg) is associated with serious adverse events such as toxic metabolic encephalopathy, it and can lead to bluish discoloration of the entire surgical field due to leakage when surgical procedures take longer [6].
On the other hand, various other imaging modalities are described, all of which have their drawbacks. Radio-guided identification using 99mTc-sestamibi and portable gamma probes do not give real-time visual guidance. In addition, nuclear isotopes are rare in large areas of the world [6].
Currently, US- guided blue dyes, especially MB injection, are used to identify parathyroid tumours. It is considered safe for humans and has fewer side effects [7].
The aim of this study was to confirm the preoperative localisation of abnormal parathyroid glands and evaluate the contribution of US-guided ultra-low-dose MB staining to the surgical performance of parathyroid tumours.
Material and methods
This was a retrospective study of 228 patients seen in our radiology, endocrinology, and general surgery clinics in the period January 2018 to December 2020.
Patients’ data were obtained from patient files. Demographic characteristics, laboratory results, and surgical and pathology reports were collected for all patients.
Preoperative biochemistry, US, and scintigraphy reports (e.g. parathyroid hormone, calcium, phosphorus, creatine, albumin, 25-hydroxyvitamin D, and 24-hour urine) were performed on all patients, and fine-needle aspiration (FNA) procedures were performed on 25 patients. CT and magnetic resonance imaging (MRI) were not needed in the study.
Inclusion criteria: patients with biochemical and clinical diagnosis of primary hyperparathyroidism, scintigraphic imaging for parathyroid adenoma, parathyroid adenoma detected by neck US, and positive FNA-PTH test results of patients were included in the study.
Exclusion criteria: patients with secondary and tertiary hyperparathyroidism, suspected ectopic thyroid lesions, or malignancy. Non-localised adenomas, hypertrophic parathyroid glands, previous neck surgery, large goitres, multiple endocrine tumours, familial hypocalcaemia, malabsorption, pregnancy or lactation, and those younger than 18 years were excluded.
Written informed consent was obtained from all patients participating in the study.
Technique
An experienced consultant radiologist performed all the applications that appear herein.
Neck US was performed using a GE Logiq E9 high-precision medical instrument with a 7.5-MHz linear array transducer. Greyscale and real-time Doppler images were obtained.
The blue dye was injected by a consultant radiologist. In each case, the supervising radiologist carefully reviewed previous images before injection to confirm the localisation of the same lesion.
Briefly, before surgery, a radiologist took a preoperative US with the patient in the supine position and the shoulders rotated to extend the neck. Once abnormal thyroid tissue was found, the neck was cleaned with povidone-iodine solution and the position of the needle tip was confirmed within the area of interest. Then 0.2 ml of 1 : 5 diluted MB solution was injected directly into the adenoma under real-time US guidance using a tuberculin syringe (1 cc) and a 26-gauge needle for injection. Typically, only one injection was given directly into the suspected adenoma. The needle was then removed from the mass, and 0.1 ml of dye was injected under the skin to guide the incision before removing it from the body.
The patient was sent to the operating room 3-5 minutes after staining with MB. During dissection, the blue helps guide the direction of dissection and the extent of resection. Minimally invasive surgery was performed under MB guidance.
All patients had successful adenoma resection. Postoperative pathology determined the adenoma, normal serum calcium levels were reached on the morning after surgery, and the patients’ serum calcium levels remained normal for 6 months postoperatively.
Statistical analysis
Data were analysed using SPSS 20 statistical software (IBM Corp., New York, USA). Continuous variables are expressed as mean ± standard deviation or median depending on the distribution of the data. Univariate logi-stic regression analysis was used to identify variables associated with MB staining results. Variables with statistically significant effects were included in the regression analysis. P < 0.05 was considered statistically significant.
Results
This was a retrospective study of 228 patients in radiology and surgery clinics. A total of 163 patients were female and 65 were male. The mean age of patients was 42.5 years (range, 25-60 years).
The patient’s clinical and laboratory findings were consistent with primary hyperparathyroidism. The patients’ medical histories were characterised by weakness, fatigue, dry mouth, hypercalcaemia, myalgia, and bone pain (Table 1).
Table 1
Clinical characteristics of the patients
| Factor | ||
|---|---|---|
| Age (years) | 25-60 | |
| Mean age | 42.5 | |
| Gender, n | ||
| Male | 163 | |
| Female | 65 | |
| Weakness and fatigue, n | 168 | |
| Muscular pain and bone ache, n | 114 | |
| Dryness of the mouth, n | 42 | |
| Hypercalcaemia, n | 85 | |
| Others, n | 87 | |
Laboratory results included in the study were: serum calcium level 11.6 ± 0.5 (8.4-10.4) mg/dl, serum phosphorus level 3.0 ± 0.3 (1.8-3.9) mg/dl, 24-hour urinary calcium excretion 273 ± 33 (100-300) mg/day, serum parathyroid hormone level 291.2 ± 33.2 (81-138) pg/ml, and FNA-PTH elution value 2443.14 ± 1131.43 (810-7528) pg/ml. In addition, serum creatine was 1.01 ± 0.2 (0.84-1.21) mg/ml. The laboratory characteristics of patients are shown in (Table 2).
Table 2
The laboratory results are given
US was performed on all patients, of whom 203 (89%) had a positive test (Figure 1), and 25 patients (11%) had a negative test, while all patients had a positive sestamibi scan (100%) (Figure 2) without the need for CT or MRI. The examinations used US-guided needle injection with MB dye, and the target tumours were successfully removed in all cases (Table 3).
Figure 1
Neck ultrasound shows well defined oval hypoechoic mass seen posterior and inferior to the lower part of the left thyroid lobe measuring 3.2 × 1.1 cm, suggesting parathyroid adenoma, confirmed by parathyroid scintigraphy in Figure 2
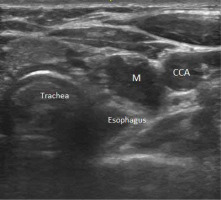
Figure 2
Parathyroid scintigraphy, 99mTC-MIBI showing evidence of persistent hot nodule is seen just inferior to the left thyroid lobe compatible with parathyroid adenoma
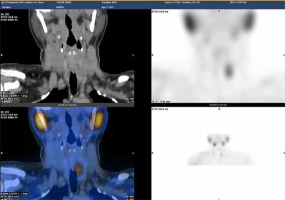
Table 3
Patients’ characteristics with various preoperative tools used to localise and identify parathyroid adenoma
| Number of patients | US | Tc scan | Methylene blue (MB) |
|---|---|---|---|
| 203 | +ve | +ve | +ve |
| 25 | –ve | +ve | +ve |
The diagnosis and localisation of suspected parathyroid adenomas were confirmed by FNA-PTH scanning in 25 suspicious cases.
In 25 cases, the tumour was not visible on US, but it was positive in scintigraphy, so a US examination was repeated for detection of the tumour.
The average diameter of the resected lesions was 18 mm (range, 12-25 mm).
All patients had positive intraoperative identification of parathyroid adenoma and MB staining (Figure 3), while surrounding tissues were unstained, e.g. thyroid, lymph nodes, and thymus (100% accuracy, 100% sensitivity, and 100% specificity).
Figure 3
Intraoperative image of the same patient in Figures 1 and 2 showing parathyroid gland after methylene blue dye injection (a blue dye-injected adenoma in situ)

In all cases, the blue dye remained long enough to be present and effective. No patient experienced permanent skin discoloration. In all cases, we found that blue dye increased visual differentiation of tissues, thus saving dissection time.
After MB staining, parathyroid adenomas were removed in all patients using minimally invasive methods. Under MB guidance, operating time (min ± SD) was 22.7 ± 11.5 (21-39) minutes. In this study, after examining the surgical and histological reports, it was found that the success rate was 100% in all patients. All cases were reported as parathyroid adenomas histologically.
The surgery was successful for all patients. Intraope-rative parathormone hormone levels decreased by more than 50% in all patients. At postoperative follow-up, hyper-calcaemia and parathyroid hormone were corrected in all patients. All patients were normocalcaemic, with a median follow-up of 9 months (range, 6-12 months).
No patient showed any signs of an allergic reaction to the MB dye injection. There were no needle-related complications such as haematoma or nerve damage. There were no complications associated with surgery (e.g. no permanent hypoparathyroidism or recurrent nerve palsy).
Discussion
For many years, bilateral neck exploration and identification of the 4 glands remained the gold standard for parathyroid surgery, and routine preoperative imaging for primary surgery was considered unnecessary [8,9]. Times have changed, and there is no doubt that advances in imaging research have changed the surgical treatment of patients with primary hyperparathyroidism and contributed to the development of new surgical techniques [10].
When the preoperative position is unclear and/or questionable, neck exploration is performed through extended surgery, which increases the risk of complications and surgical failure [11].
With advances in preoperative localisation research and increased public demand for minimally invasive surgery, new techniques targeting the parathyroid glands have been described and applied over the past 20 years [12].
Since the success of the limited approach depends largely on accurate preoperative localisation, surgeons rely heavily on the quality of preoperative localisation to choose the focused approach wisely [10].
Ultrasonography and 99mTc-sestamibi scintigraphy are essential imaging techniques for preoperative localisation of parathyroid adenoma. Several studies comparing these techniques have shown similar sensitivity and specificity for detecting solitary adenoma. Localisation accuracy also improves when both studies are obtained preoperatively [13]. CT and MRI are also effective in localising parathyroid adenomas, but they are used less frequently for pre-operative localisation and more commonly in determining failure of parathyroidectomy to detect suspected ectopic glands (usually mediastinal glands). CT is rarely used if the results of US and 99mTc-sestamibi scintigraphy are discordant [14].
US-guided injection of MB was also used before surgery to localize thyroid tumours.
This technique has been applied to parathyroidectomy by Harari et al. [15] and Candell et al. [16], who reported the first case series using US-G blue dye injection to determine the site of parathyroidectomy.
We used blue dyes, specifically MB, to localise parathyroid adenoma. It is considered safe for humans and has no side effects. We and others have used a 1 : 5 dilution of dye without any significant reduction in efficacy. We should emphasise that we inject before incision to prevent dye washout from the tissue, although this cannot be done quickly [16,17].
The main reason for staining parathyroid adenomas with MB was to distinguish parathyroid adenomas from thyroid nodules and lymph nodes before surgery to ensure the diagnosis and localisation of adenomas, which is consistent with Abdel-Ghani’s view [18].
We successfully identified and removed abnormal parathyroid glands in all patients without any complications. Previous studies of parathyroidectomy have shown that 10-20% of patients develop permanent hypoparathyroidism and 3-10% develop recurrent laryngeal nerve palsy [19,20]. Pate et al. [21] administered intravenous MB, which stains the gland blue and facilitates visual identification of enlarged parathyroid glands. The surgical area can also be dyed blue using this method. Blue staining of other tissues may lead to surgical failure and is neurotoxic at high doses.
We should mention that the tumours we injected were small (ranging from 12 to 25 mm in diameter), and this technique would be very useful in this group of patients, as identifying small tumours can be very difficult, which is consistent with Thabet et al. [22].
The present study demonstrates that the MB staining method is useful in localisation and surgical intervention. The MB staining method combined with preoperative US guidance provides accurate information on the localisation of parathyroid tumours. In this setting, focused surgical intervention of parathyroid lesions guided by MB can be successful in a very short time. The results are consistent with Bui et al. [23].
In a previous study, it was reported that FNA-PTH washout is useful in differentiating between parathyroid adenomas and posterior thyroid nodules, and in diagnosing and localising parathyroid incidentalomas [24], and our study is consistent with this.
Giusti et al. [25] showed that the FNA-PTH washout method could detect the diagnosis and localisation of suspected thyroid tumours with high diagnostic sensitivity and specificity, which is consistent with our study.
Orlov [26] found that the sensitivity and specificity of MB staining were 79% and 93%, respectively, and when evaluating histopathological data, the diagnosis, localisation, and surgical resection of parathyroid adenoma using this method has 100% sensitivity and 100% specificity.
US examination was performed in all patients, and 203 (89%) patients were positive, which was more than in the study of Lumachi et al. [27]. US is used as the first line of thyroid imaging for several reasons. The procedure is simple, quick, and well tolerated by patients. It does not require the use of contrast media and does not emit radiation. It provides good anatomical information about neck masses and can identify 95% of adenomas when performed by experienced radiologists. Furthermore, it is the cheapest preoperative localisation technique.
US sensitivity depends on the operator, material, and size. The detection limit is approximately 5 mm [28].
We did not perform other additional imaging, such as CT and MRI, because parathyroid CT is relatively expensive, exposes patients to radiation, and requires the use of contrast media. It has a false positive rate of up to 50%. CT has been shown to have a sensitivity of 67% [10]. MRI is expensive, and patient compliance is sometimes limited due to claustrophobia. The sensitivity rate is 88% [29]. Henry et al. noted that MRI is often reserved as a second-line examination for localisation during re-operative thyroid surgery when US and sestamibi scanning fail to identify an abnormal thyroid gland that may be located in the mediastinum [10].
Gotthardt et al. report of parathyroid imaging using Technetium-99m methoxy isobutyl isonitrile (sestamibi). Sestamibi is often localised to parathyroid adenomas, but the exact mechanism remains controversial. High mitochondrial activity is the major component of sestamibi uptake by human parathyroid tissue in patients with primary hyperparathyroidism. Reported sensitivity is 90%. Reported allergies vary widely [30].
Our high success and complication-free rates are directly related to the use of neck US, 99mTc sestamibi scinti-graphy, and US-guided dye injection as preoperative localisation studies, which is consistent with Sugino et al. [31].
All patients underwent successful surgery. During surgery, parathyroid hormone levels decreased by more than 50% in all patients. At a median postoperative follow-up of 9 months (range 6-12 months), hypercalcaemia and parathyroid function were corrected in all patients, and serum calcium levels were normal in all patients, which is consistent with Candell et al. [16].
Conclusions
US-guided blue dye injection is a safe, simple, and useful tool when performing parathyroidectomy, even in small parathyroid gland adenoma. The localisation of MB dye aids in the identification and successful removal of these small parathyroid adenoma. There were no systemic or local complications associated with dye injection.






