Dear Editor,
I am writing to discuss a pertinent issue in radiological practice: whether beta-human chorionic gonadotropin (β-hCG) testing should be routinely performed in women of childbearing age before undergoing computed tomography (CT) imaging. This topic has significant clinical, ethical, and operational implications.
The primary concern in this context is the potential for inadvertent foetal radiation exposure during early pregnancy, particularly in cases where pregnancy may be unrecognised. While the risk of teratogenic effects at diagnostic CT doses is minimal, the precautionary principle often prevails in clinical decision-making, emphasising the importance of confirming pregnancy status to mitigate potential harm [1].
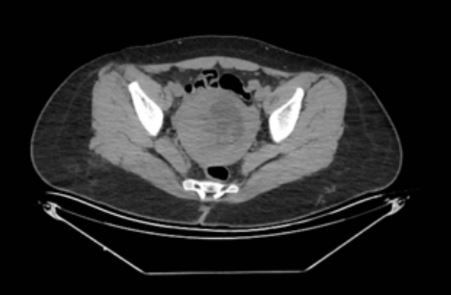
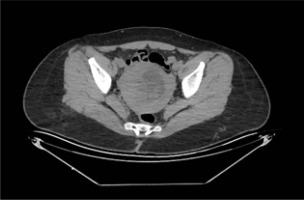
A patient, unaware of her pregnancy, presented to the emergency department with complaints of abdominal pain and underwent an abdominal CT scan. As seen in Figures 1 and 2, it was subsequently determined that the patient was pregnant, and she was referred to the obstetrics clinic. It was later established that the patient was 10 weeks pregnant and had not attended regular follow-ups. At 25 weeks of pregnancy, the patient was admitted to the emergency delivery ward due to cervical dilation of 5-6 cm. However, the patient left the ward without permission before completing the labour process.
Routine β-hCG testing prior to CT, however, is not without its challenges. First, the prevalence of unrecognised pregnancies in the population undergoing imaging must be considered. Studies suggest that a relatively small proportion of imaging referrals in women of reproductive age involve unrecognised pregnancies [2]. Second, the urgency of many CT indications, such as trauma or suspected pulmonary embolism, often precludes the time required for laboratory confirmation of pregnancy status [3]. Delays in diagnosis and treatment in such cases may pose a greater risk to maternal and foetal outcomes than the theoretical risks of radiation exposure [4].
Moreover, the financial and logistical burdens of routine β-hCG testing cannot be ignored. Instituting a universal testing protocol for all women of childbearing age may strain healthcare resources without clear evidence of benefit, particularly in low-risk populations. An alternative approach may involve targeted testing based on clinical history, symptoms, and imaging necessity, supported by robust counselling regarding the risks and benefits.
In conclusion, while routine β-hCG testing before CT has theoretical merit, its implementation should be guided by evidence-based risk stratification and clinical urgency. Further research is needed to evaluate the cost-effectiveness and clinical outcomes of universal versus selective β-hCG testing strategies.
I hope this correspondence fosters further dialogue and research on this important topic, ultimately guiding best practices for safe and effective imaging in women of childbearing age.