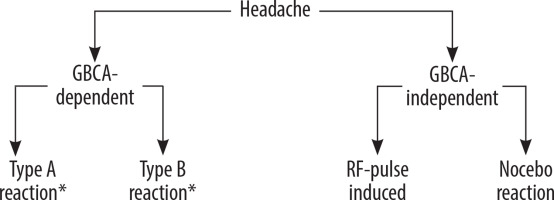
Magnetic resonance imaging (MRI) is a popular imaging modality because it works without ionizing radiation and has an excellent spatial resolution [1]. Usually, patients tolerate MRI very well. Nevertheless, adverse events do occur even in patients undergoing MRI. Although headache is a common [2], unwanted reaction in the context of a MR-scan, there is sparse information about it in the literature. Headache occurs either dependent on or independent of the application of gadolinium-based contrast agents (GBCA) (Figure 1). Because the clinical differentiation of these forms can be difficult, the goal of this publication is to help to find the correct diagnosis. Based on the correct diagnosis, preventive or therapeutic measures can be introduced.
Figure 1
Classification of the pathology of headache in patients undergoing contrast-enhanced MRI. There are two groups, gadolinium-based contrast agent (GBCA) dependent and independent (for detailed information see [5])
If headache occurs during non-contrast-enhanced MRI, it is reasonable to suspect that it could be due to influences from the magnetic field. However, the situation is more complex for patients who received a GBCA. In such cases, both the contrast medium and the magnetic field can be responsible for the patient’s headache. The responsible radiologist should be aware of this fact. How can we differentiate between GBCA-induced and RF pulse-induced headache forms? Generally, most non-contrast MRI sequences will be obtained before injection of GBCA. Patients who have GBCA-related headache will be symptom-free in this situation. Patients who are already sensitive to RF pulses are likely to complain of headaches in this situation. Nocebo-related headaches should also be considered in the differential diagnosis. We should realize that nocebo-related headache can occur during both contrast media (CM)-enhanced and CM-non-enhanced (naïve) MRI.
Why do we need an exact differentiation of the cause of headaches during a MRI-scan? Depending on the cause, we must carry out an appropriate prophylaxis.
If it is a patient with GBCA-induced headache, switching to another substance (i.e. a non-culprit GBCA) as prophylaxis should make sense. Painkillers are helpful for radiofrequency (RF)-pulse-induced headache forms. Nocebo-related headaches might cause unnecessary use of painkillers. Distinguishing between nocebo- and GBCA-induced headache is difficult. Naive MR imaging may be able to help. Sometimes a detailed doctor-patient talk is also useful as prophylaxis in such cases.
Headache in patients undergoing contrast-enhanced MRI is a common side effect. There are at least four different reasons for this kind of adverse reaction (Figure 1). Adverse reactions in the context of contrast-enhanced imageguided examinations may be either contrast dependent or independent [3]. Contrast-dependent reactions are either type A or B reactions [4].
GBCA-independent headache may be due to magnetic fields. Usually, medical staff working in MR-scanner rooms acquire subjective symptoms such as headache, tinnitus, nausea, warm/hot feeling, dizziness, vertigo, feeling lightheaded or weightless, concentration problems, metallic taste, and a feeling of instability when standing or moving [5]. MRI-related electromagnetic fields (EMFs), static magnetic fields (SMFs), and switched gradient fields (SGF) seem to be responsible for the symptoms [5]. Controversially, even the RF pulse might induce headaches [2]. Therefore, adverse reactions to RF pulses could occur in patients. Due to the sparseness of data, it would be desirable if there were corresponding studies on this topic, although this is a very rare event. RF-pulse-induced headache is independent of the contrast agent used. Consequently, such an adverse event is not a hypersensitivity reaction. Moreover, headache during a MR-scan might occur due to the volume or pressure of the headphones used for noise protection, continued noise during examination upon insufficient protection, or associated with a head-coil.
Conclusion: Taken together, headache in patients undergoing MR scans may have different causes. Besides GBCA-related forms, there are also GBCA-independent forms, which may be RF-pulse triggered (Figure 1). Therefore, when observing adverse reactions following the injection of a CM, the following recommendations are made: 1) to make an exact clinical diagnosis, 2) to identify the culprit substance/factor, and 3) to exactly document all facts (i.e. date of the adverse reaction, culprit factor, and clinical symptoms) [6]. An exact differentiation is necessary with respect to the treatment or prophylactic actions in future MR scans. In cases of GBCA-induced headache, the change to a non-culprit compound is the prophylaxis of choice, and in cases with GBCA-independent headache, RF-pulse-induced forms should either be verified or excluded.


