Introduction
Chronic otitis media (COM) is a significant medical problem, affecting approximately 2% of the population [1]. It is defined as chronic inflammation of the lining of the middle ear with perforation of the tympanic membrane, persistent or temporary ear discharge, and hearing loss. This disease can occur in various forms – both active, i.e., with discharge from the ear (simple COM, COM with granulation, COM with cholesteatoma, and COM in specific diseases), and inactive, i.e., without discharge (dry perforation of the tympanic membrane, atelectasis, tympanosclerosis, and adhesive otitis media). From a clinical perspective, cholesteatoma is the most dangerous form [1-8].
Otitis media with cholesteatoma always requires surgical treatment. Currently, the most commonly performed procedures use the closed technique (canal wall up – CWU), which preserves the ear’s anatomy and thus its waterproofness and self-cleaning after the surgery. Less frequently, usually in selected cases, open technique surgeries (canal wall down – CWD) are performed, which significantly interfere with the structure of the middle ear and result in a large postoperative cavity that needs protection from water and regular cleaning. These procedures (CWU and CWD) are sometimes combined with mastoid obliteration. With both types of surgery, there is a significant risk of cholesteatoma recurrence (recurrent and residual), which is 2-3 times higher with the closed technique than with the open technique [9,10]. Van der Toom et al. [10] reported that the combined rate of recurrent and residual cholesteatomas after 5 years of follow-up in 337 adult patients was 34.9% in the CWU group and 17.9% in the CWD group.
While otoscopic examination is almost always sufficient to control the postoperative cavity after CWD tympanoplasty, it is not suitable for patients who have undergone a closed-technique surgery. In the past, every patient who underwent a CWU surgery for cholesteatoma needed a second-look operation one year after the first procedure, to detect residual or recurrent disease. Nowadays, this is increasingly being replaced by magnetic resonance imaging (MRI) of the head with the diffusion weighted imaging without echo-planar imaging (DWI non-EPI) sequence, which can detect cholesteatomas as small as 3 mm in diameter [11,12]. Choi et al. [12] demonstrated that MRI DWI non-EPI not only avoids potential risks and complications associated with ear reoperation, such as facial nerve damage, hearing loss, infection, bleeding, or the need for general anaesthesia, but also significantly reduces healthcare costs.
The aim of this study was to evaluate the effectiveness of head MRI with the DWI non-EPI sequence in detecting cholesteatoma recurrence, with a particular analysis of false results.
Material and methods
Study design
This was a retrospective study conducted in a tertiary referral clinical centre. The study included patients who were diagnosed with cholesteatoma and underwent surgical treatment performed by experienced otosurgeons. Patients with incomplete medical records and those who did not undergo a preoperative MRI were excluded from the study.
Patients
The analysis included 156 patients who underwent middle ear reoperation in the clinical department between 2015 and 2021. All these patients had previously undergone a surgery for cholesteatoma in the same ear. Each patient underwent an MRI scan of the head with the DWI non-EPI sequence before the reoperation. Indications for reoperation included suspected cholesteatoma recurrence on the MRI or otoscopic examination, as well as tympanic membrane perforation or conductive/mixed hearing loss (with preserved air-bone gap) qualifying for myringoplasty or ossiculoplasty. The group consisted of 80 men (51%) and 76 women (49%). The average age of the patients was 40.4 years (range 11-83 years).
Methods
The following medical records were analysed: 1) protocols from middle ear surgery and reoperation, 2) medical histories and outpatient records, and 3) imaging results (temporal bones computed tomography [CT], head MRI with DWI non-EPI sequence). The MRI scanner used was a 1.5T Magnetom Aera MRI scanner from Siemens Healthineers. All MRI scans were independently evaluated by experienced radiologists and otosurgeons. In cases of disagreement, which occurred occasionally, the assessments were discussed and resolved collaboratively.
Results
Concordance of clinical and radiological findings (true positive and true negative results) was found in 80% of patients. True positive results, indicating the presence of cholesteatoma on MRI and intraoperatively, were observed in 77.5% (121/156) of patients, while true negative results, indicating the absence of cholesteatoma on MRI and intraoperatively, were found in 2.5% (4/156) of patients.
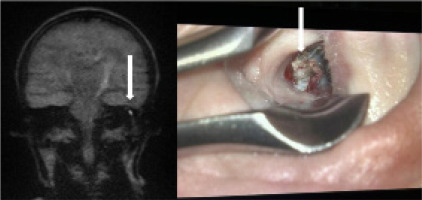
False positive results (presence of cholesteatoma on MRI, absence of cholesteatoma intraoperatively) were obtained in 8% (13/156) of patients, with the main cause being wax in the improperly cleaned external auditory canal before the MRI examination (Figure 1).
Figure 1
Patient after canal wall up (CWU) cholesteatoma surgery. Cerumen-epidermal deposits in the left external auditory canal visible on magnetic resonance imaging (suggesting cholesteatoma recurrence) and during otoscopy (indicated by white arrow)
False negative results (absence of cholesteatoma on MRI, presence of cholesteatoma intraoperatively) were obtained in 12% (18/156) of patients, with almost three-quarters of these results due to the presence of mural cholesteatoma (Figure 2) or cholesteatoma with a small diameter (approximately 2 mm) (Figure 3).
Figure 2
Patient after canal wall up (CWU) cholesteatoma surgery. Mural cholesteatoma of the left middle ear, which was not detected by magnetic resonance imaging but was visible during surgery (indicated by white arrow)
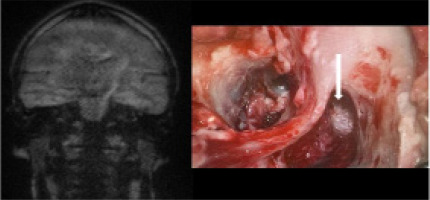
Figure 3
Patient after canal wall up (CWU) cholesteatoma surgery. A 2 mm cholesteatoma in the right middle ear, which was not detected by MRI but was visible during surgery (indicated by white arrow)

Statistical analysis revealed no significant association between the MRI DWI non-EPI results and intraoperative findings (p = 0.415676).
The sensitivity (ratio of true positive results to the sum of true positive and false negative results) of the MRI DWI non-EPI examination in detecting cholesteatoma was 87%.
The positive predictive value was 90.3%, meaning that when the MRI result is positive, there is a high likelihood of the presence of cholesteatoma. However, the low negative predictive value [NPV] of 18.2% indicates that a negative MRI result does not effectively exclude the possibility of cholesteatoma.
A detailed analysis of false positive and false negative results is presented in Tables 1 and 2.
Discussion
Although otoscopic examination remains the primary diagnostic tool for COM, radiological imaging (CT, MRI) has also played an important role for many years. CT imaging visualises the bony structures of the middle ear very well, allowing precise localisation of pathological masses and visualisation of erosion of the ossicles, facial nerve canal, or labyrinth fistula. However, it is unable to differentiate between individual pathological lesions such as mucosal oedema, granulation tissue, cholesteatoma, postoperative scars, or cholesterol granuloma [5,7,12-20]. MRI, on the other hand, enables a precise evaluation of soft tissues, allowing differentiation between cholesteatoma and other middle ear pathologies. This is clinically significant, especially for monitoring patients who have undergone surgery for cholesteatoma. In the last decade, some otosurgical centres have also performed fusion of temporal bone CT imaging with MRI DWI non-EPI. This allows for a more precise localisation of the cholesteatoma in relation to anatomical landmarks of the middle ear, and facilitates intraoperative identification and removal of the pathological lesion by the surgeon [15-20].
In MRI, the EPI DWI trajectory used by conventional DWI makes such sequences prone to substantial susceptibility artifacts, and single-shot EPI sequences were found to be poor at identifying lesions of 4-5 mm. Consequently, non-EPI DWI techniques began to be favoured; such algorithms minimise susceptibility artifacts and geometric distortion related to the skull base and can detect lesions as small as 2 mm. BLADE (Siemens) and other sequences (such as PROPELLER) are subtypes of non-EPI techniques that minimize susceptibility artifacts and geometric distortions by sampling k-space [18,19].
We suggest shortening the protocol for monitoring cholesteatoma: 1) T2 TSE axial, 2) T2 TSE coronal 2 mm, 3) non-EPI DWI thin-section coronal multi-shot 20 slides; TR 3000 ms; TE 82.44 ms; thickness 3.00 mm; inter-slices gap 0; FA 90; view size 1168 × 1230; matrix 152 × 152; b = 0 and b = 800 s/mm2. We do not recommend the contrast injection. The examination may be aimed at excluding recurrence or may constitute an extension of the MRI examination of the head in a patient after a cholesteatoma surgery. In such cases, we recommend adding only the non-EPI DWI sequence to the routine examination.
In our study, the sensitivity of MRI DWI non-EPI in detecting cholesteatoma was 87%, which was similar to that described in the literature. Amoodi et al. [21] and Jindal et al. [22] in their studies, which were large systematic reviews of the literature, described high sensitivity of MRI DWI non-EPI, with values of 92.2% and 91%, respectively. Meanwhile, Piekarek et al. [23] in a study involving 32 patients with suspected COM with cholesteatoma demonstrated the superiority of the DWI non-EPI sequence over the DWI EPI sequence in cholesteatoma diagnosis. The sensitivity and specificity were 100% vs. 69.2% and 83.3% vs. 66.6%, respectively.
Our analysis revealed 13 false positive results, with most being wax-keratin masses in the external auditory canal. All these patients were previously instructed to undergo ear cleaning before the imaging examination at a regional ENT clinic. Follow-up visits at our centre took place with the MRI results. During these visits, wax masses in the external auditory canal were removed after reassessment. In cases where reconstructive surgery of the tympanic membrane or ossicles was indicated, the patient was subjected to myringoplasty and/or ossiculoplasty. During these surgeries, the absence of cholesteatoma within the middle ear was confirmed. For patients ineligible for reconstructive surgery, the MRI examination was repeated after a careful ear cleaning in our department. Another observation in our study is that the highest number of false positive results occurred in the initial years after the introduction of MRI with the DWI non-EPI sequence for cholesteatoma diagnosis in our centre. Between 2015 and 2018, this number was 9 out of 74 (12%) examinations conducted, whereas between 2019 and 2021 it was 4 out of 82 examinations (5%). The experience of both the otosurgeon and the radiologist contributed to the decrease in this number in the subsequent period. On the one hand, this resulted from the change in approach and having the ears cleaned under a microscope each time in our centre. On the other hand, it was the effect of the increased experience of both radiologists and otosurgeons in evaluating cholesteatoma using the DWI non-EPI sequence. Benson et al. [24] mentions in his paper that wax, abscess, and brain herniation may yield false positive results. Therefore, in cases of suspected brain herniation, simultaneous evaluation of the non-EPI DWI sequence and the thin-slice T2 CISS sequence is emphasised. Additionally, Balik et al. [16] and Dremmen et al. [17] described in their studies that empyema can imitate cholesteatoma on MR DWI non-EPI. Furthermore, the fat used in the previous surgery to fill the postoperative cavity can yield a high signal on DWI sequences [17]. Meanwhile, Muhonen et al. [14] described that cartilage grafts may cause restricted diffusion on the DWI sequences. Recent research also highlights the complexities in detecting residual cholesteatoma with MRI-DWI. According to a study by Eggink et al. [25], four cases had false positive MRI-DWI results: one due to a previously placed Silastic™ sheet, two cases with ear wax accumulation, and one case with no unusual findings.
It is also important to consider the possibility of false negative results. In our study, the majority of these were caused by the presence of small-sized and mural cholesteatomas. These cholesteatomas were detected in some patients who underwent surgery to close tympanic membrane perforations or improve hearing. A retrospective study by Balik et al. [16] conducted on a group of 39 patients with cholesteatoma described a lesion with a diameter of 2 mm being responsible for a false negative case. Similarly, Horn et al. [26], Geoffray et al. [27], and Vercruysse et al. [15] described in their studies that cases of false negative results involved cholesteatomas smaller than 5 mm and mural cholesteatomas. Therefore, it is standard procedure in our centre to repeat the MRI DWI non-EPI examination 3 and 5 years post-surgery in patients who show no signs of cholesteatoma recurrence in the MRI examination conducted one year after surgery and do not require ear reoperation for reconstruction. Moreover, a case report by Fong et al. [20] demonstrated that, although titanium is an MRI-compatible material, the presence of titanium within or near cholesteatoma may reduce the NPV of MRI DWI non-EPI as a screening tool. For this reason, surgeons and neuroradiologists should be aware that a negative MRI result in patients with titanium prostheses should be interpreted with caution. In such cases, second-look surgery may still be indicated, even in the presence of a negative result on MRI. What is more, the study by Eggink et al. [25] suggested that children have a higher rate of false negative MRI-DWI results, which could be attributed to the specific growth pattern of paediatric cholesteatoma – this type of cholesteatoma tends to be more invasive and does not form dense keratin pearls with associated diffusion restriction.
Conclusions
MRI DWI non-EPI is a valuable and effective tool for detecting cholesteatoma recurrence, which in many cases allows the avoidance of unnecessary second-look surgery. However, it is important to be aware of the possibility of false positive and false negative results. Each result obtained should be correlated with the clinical examination. The simplest way to reduce the number of false positive results is to carefully clean the ear under a microscope shortly before the MRI examination. On the other hand, to reduce the number of false negative results, it is necessary to repeat the MRI DWI non-EPI examination several times at appropriate intervals, i.e. 1, 3, and 5 years after surgery.



