Introduction
Large and wide-necked bifurcation aneurysms remain technically challenging to treat by the endovascular approach. The pCONus stent (Phenox) is a stent-like endovascular device aiding retention of coils within wide-necked bifurcation aneurysms. We report a fatal case of treatment of a large unruptured cerebral aneurysm of the middle cerebral artery using a pCONus stent and coils followed by repeating enlargement, recanalisations, and subarachnoid haemorrhages.
Case report
A 64-year-old, non-smoking woman, treated for hypertension manifesting with headaches and vertigo, underwent CT angiography of the head, in which three aneurysms were detected. She was referred to planned endovascular embolisation and prepared with dual antiplatelet therapy (DAPT) for seven days before the procedure. The 3D digital subtraction arteriography (DSA) confirmed three brain aneurysms, as described in Table 1.
Table 1
Characteristics of the patient’s aneurysms
The decision to perform left middle cerebral artery (LMCA) aneurysm embolisation was taken. Because of the large neck and M2 branches arising from the dome of an aneurysm posing a risk of coil protrusion, the pCONus 4-20-10-F stent (Phenox) was positioned and detachable coils were implanted into the aneurysmal dome (Figures 1A, B). Due to the complex morphology of the aneurysm and the repeating coil protrusion, the coiling implantation was stopped before complete obliteration was achieved. The pCONus device was then detached and control angiography confirmed the flow of all arising branches and contrast opacification within the coil interstices of a residual aneurysm (Modified Raymond-Roy classification – 3A). Postoperatively the patient did not show any symptoms of neurological dysfunction, DAPT was continued, and the patient was scheduled for the right middle cerebral artery (RMCA) embolisation in three months and discharged. DAPT was continued for three months and then only aspirin (150 mg) was administered.
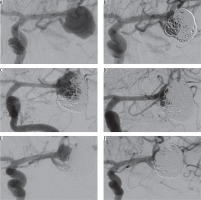
Figure 1
A) Wide-necked left middle cerebral artery aneurysm before embolisation; pCONus is positioned at the neck. B) Immediate angiographic control after first embolisation shows a remnant aneurysm with contrast agent inside the sac. C) Angiography after 13 months shows compression of coils and recanalisation of an aneurysm. D) Immediate angiographic control after second embolisation – the dome of an aneurysm filled with an additional 7 coils. E) Arteriography after 16 months (second SAH) shows once again the coil compression with recanalisation of an aneurysm. F) Immediate angiographic control after third embolisation with 7 additional coils – complete exclusion of the dome with the neck remnant
Three months later the patient was readmitted. The RMCA aneurysm was embolised with detachable coils and was completely excluded from the circulation with preservation of the blood flow in the parent vessels, with no complications during or after the procedure. The LMCA aneurysm was controlled and showed subtle coil compression compared to the previous angiography. The patient was scheduled for second-stage treatment of the LMCA aneurysm but refused to be admitted to the hospital due to family reasons.
One year after LMCA aneurysm embolisation the patient was admitted for control DSA, which showed the complete obliteration of the RMCA aneurysm and enlargement of the LMCA aneurysm with recanalisation and compression of coils. The woman was once again scheduled for second-stage treatment of the LMCA aneurysm.
One week before the planned second-stage embolisation, she was readmitted due to subarachnoid haemorrhage (SAH). On examination, the patient was conscious, in logical verbal contact, and with positive meningeal symptoms and right hemiparesis – Hunt and Hess scale score of 3. CT of the head revealed SAH with hyperdense blood localised mainly in the left hemisphere grooves. The urgent DSA revealed enlargement and recanalisation of the LMCA aneurysm with coil compression compared to the previous examination (Figure 1C). The dome of the remaining sac was completely filled with detachable coils, and the aneurysm was excluded from the circulation, retaining blood flow in the parent vessels. Adequate occlusion was achieved with dome embolisation and neck remnant. There were no technical or neurological procedure-related complications. The slight right hemiparesis retracted, and the patient was discharged with clinical improvement (Hunt and Hess scale score of 1).
Three months after last hospitalisation the patient was urgently readmitted diagnosed with SAH from a ruptured aneurysm of the LMCA, in severe condition, unconscious, intubated, on assisted breathing, neurologically manifesting anisocoria, and right-sided hemiparesis. CT of the head showed SAH and large intracerebral haemorrhage surrounding the embolised aneurysm in the left fronto-temporo-parietal region with mass effect, displacement of the middle structures to the right side, and the presence of blood in the ventricular system. Emergency neurosurgical decompression of the intracerebral haematoma was performed, followed by embolisation of the LMCA aneurysm. DSA showed again enlargement and coil compression with recanalisation of the aneurysm. The remnant part of the aneurysm sac was 9 × 12 mm (Figure 1E). Embolisation of the LMCA aneurysm was performed immediately with detachable coils, achieving a similar result to the previous procedure, with a complete exclusion of the dome with the neck remnant (Figures 1F and 2). After the procedure the patient remained in a serious condition – unconscious and intubated. During further hospitalisation the patient did not require any surgical re-intervention. In severe condition she was transferred to the intensive care unit in her local hospital where she eventually died. A summary of the procedures and time at which the patient received them is shown in Table 2.
Table 2
Time and characteristics of procedures the patient underwent
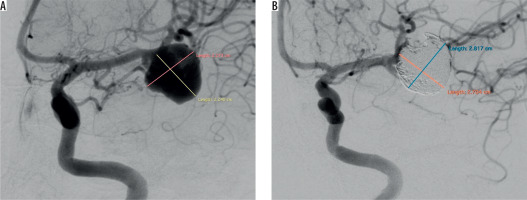
Figure 2
Comparison of size of left middle cerebral artery (LMCA) aneurysm before first and after last embolisation. A) Wide-necked LMCA aneurysm before embolisation (22.73 × 22.40 mm). B) LMCA aneurysm after last embolisation (28.17 × 27.04 mm). Significant difference in size of the aneurysm is visible
Discussion
Several endovascular strategies have been established in recent years for the treatment of wide-necked bifurcation aneurysms, such as balloon-assisted coiling, stent-assisted coiling, waffle cone technique (WCT), and intrasaccular flow disruptors. The pCONus stent is dedicated to WCT: it consists of stent-based support for the proximal part of the parent vessel with clover-shaped petals creating an effective scaffold for the aneurysm. Current endovascular treatment with the pCONus is reported to be an effective therapeutic option for managing patients with wide-necked bifurcation aneurysms [1-4].
The physicians that performed the embolisation have extensive experience in using the pCONus stent; they introduced the novel technique of combined use of a pCONus and a Solitaire stent for the treatment of complex intracranial aneurysms [5]. We believe that the treatment decisions were correct because the team ensured frequent control of the patient, and when it became clear that there was a need for second-stage embolisation the patient was immediately scheduled. Unfortunately, the woman could not be admitted due to personal reasons, and when the woman was scheduled for the second time, unfortunately, she developed SAH one week before admission to hospital. The second embolisation ended with neck remnant, although the dome was fully occluded, but it did not prevent the aneurysm from enlargement and rupture in the region between the distal end of pCONus stent and coil mass. Our team was surprised with the unfortunate outcome of treatment – it contributed to the authors’ decision to search for similar cases in the literature and to publish this one.
There are suggestions that the use of a pCONus stent may change in some cases the haemodynamic situation by directing the bloodstream toward an aneurysm instead of diverting it [6,7]. This theory was not confirmed by Pérez et al. [8] in their in vitro study. On the other hand, there are similar reports of complete aneurysm occlusions assisted with a pCONus stent, which showed residual aneurysm perfusion and aneurysm enlargement in the follow-up DSA [9,10]. Aneurysm size (≥ 10 mm) and incomplete initial occlusion are two major predictive factors of aneurysm recanalisation, and after first intervention both were present in our patient when the first SAH occurred but not in the second case of SAH [11-13]. We cannot exclude that concurrence of all of these factors may have contributed to the recurrent expansions and ruptures of an LMCA aneurysm.
Conclusions
Large, wide-necked bifurcation MCA aneurysms are often treatable with a pCONus stent and coils. In cases when an aneurysm is initially not fully occluded, this technique may not prevent rupture and could promote coil compaction and aneurysm enlargement, leading to severe complications. On the basis of the presented case, we would like to emphasise the importance of sufficient initial coil packing and frequent control of the neck region of the aneurysm for the long-term stability and safety after pCONus-assisted coiling of intracranial aneurysms.


