Introduction
The thoracolumbar region (T11-L1) is the most frequently injured area of the spine, with a 6.9% incidence of fractures and fracture-dislocations in blunt trauma patients [1]. The annual incidence of thoracolumbar (TL) fractures is approximately 30 per 100,000 individuals when osteoporotic fractures are included [2]. In young individuals, TL fractures are most often due to motor vehicle collisions and high-energy falls, while low-energy trauma is responsible for most fractures in elderly people [1,2]. The prevalence of these injuries is increasing, and they are associated with a relatively high mortality rate among older men [2].
TL fractures can be difficult to diagnose on clinical examination alone – only 48% to 75% of clinically significant injuries are identified during a physical exam [3,4]. Plain radiographs (X-rays), which are widely available and inexpensive, have long been accepted as a primary diagnostic tool for detecting TL fractures, mainly because they allow spinal surgeons to quickly assess spinal alignment. However, recent guidelines provide differing recommendations regarding the role of X-ray in diagnosing TL fractures. Both the NICE (2016) and ESTES (2023) guidelines allow for the use of plain radiographs as a first-line diagnostic tool in stable minor trauma patients without neurological abnormalities [5,6]. In contrast, trauma protocols in the United States and the Korean guidelines (2017) recommend performing computed tomography (CT) regardless of the trauma mechanism, due to the low diagnostic accuracy of plain radiographs [7,8]. Several studies have reported low sensitivities of X-ray for detecting TL fractures, as well as difficulties in distinguishing burst from compression fractures [9-12].
Patients with rigid spine conditions are more susceptible to spinal fractures, which may go unnoticed due to pre-existing back pain, discrepancies between reported pain locations and the actual fracture site, and a lack of trauma history [13,14]. In this population, fractures can be obscured on plain radiographs due to the distortion of anatomical structures (e.g. scoliosis, severe kyphosis, ossified spinal ligaments, or osteopenic bone) [15]. Reportedly, between 15% and 41% of rigid spine patients have a delayed diagnosis [16,17].
The aim of this study was to assess the diagnostic value of radiographs in detecting acute TL spine fractures in minor trauma patients, using CT as the reference standard. Additionally, the study aimed to evaluate how the presence of a rigid spine and the experience level of interpreting readers influence diagnostic performance.
Material and methods
This single-centre retrospective study was approved by the Institutional Ethics Committee (AKBE/188/2022), and the patients’ informed consent was waived.
Study group identification
Medical records of patients who presented to the emergency department (ED) with TL spine fractures between July 2014 and December 2020 and underwent CT were retrieved from the Hospital Information System. Two attending radiologists, each with more than 10 years of experience in musculoskeletal radiology, performed a consensus reading of the CT scans to confirm the presence of fractures and classify them according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) TL classification system [18].
Patients with acute TL spine fractures due to minor trauma, who underwent both radiography (anteroposterior and lateral views) and CT, were included in the study. Fractures were classified as acute if symptom onset occurred within 6 weeks of presentation and if CT images demonstrated cortical disruption, trabecular impaction, or thickening of the prevertebral soft tissues [19]. Minor trauma was defined as a fall from standing height or less than one meter, a mild motor vehicle collision (e.g. fender bender or rear-end collision), or the sudden onset of back pain during daily activities (e.g. lifting a heavy object or bending).
Patients with pathologic fractures, insufficiency fractures due to metabolic bone diseases other than osteoporosis, or history of prior spine surgery were excluded from the study.
From patients fulfilling the abovementioned inclusion criteria, 2 age- and sex-matched groups were selected: a rigid-spine group (patients with ASDs and fractures involving fused spinal segment or immediately adjacent non-fused spinal segment) and a non-rigid-spine group.
Blinded radiographs were evaluated independently by a fourth-year radiology resident and an attending radiologist with 10 years of experience in musculoskeletal radiology working in a spine trauma centre. The readers were asked to record spinal levels they deemed to represent acute vertebral fractures. Missed fractures were subsequently analysed for type, morphology, and displacement.
Statistical analysis
Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated. A Cohen κ coefficient was used to measure the interobserver variation between the resident and the attending radiologist. The degree of agreement was classified as follows: poor (κ < 0), slight (κ: 0.00-0.20), fair (κ: 0.21-0.40), moderate (κ: 0.41-0.60), substantial (κ: 0.61-0.80), or almost perfect (κ: 0.81-1.00) [20].
Results
Thirty-two rigid-spine (28 diffuse idiopathic skeletal hyperostosis [DISH] and 4 ankylosing spondylitis [AS]) and 31 non-rigid-spine patients were included in the radiograph-CT comparison analysis (Table 1). Among the total 63 patients, CT demonstrated 84 fractures: 49 in the rigid-spine group and 35 in the non-rigid-spine patients. Twenty-five patients had chronic vertebral deformities due to osteoporosis/previously healed fracture: 13 in the rigid-spine group and 12 in the non-rigid-spine group. Fracture distribution and morphology are presented in Tables 2 and 3. Analysed radiographic images included 42 spine series (19 lumbar, 3 thoracic, and 10 TL) in rigid-spine patients and 37 spine series (22 lumbar, 3 thoracic, and 6 TL) in non-rigid-spine patients. A spine series was comprised of 2 standard projections (AP and lateral views) of one spinal region.
Table 1
Patients’ demographics
Table 2
Fracture distribution on computed tomography
| Spinal region | Fracture number, n (%) | |
|---|---|---|
| Rigid-spine group | Non-rigid-spine group | |
| Thoracic | 11 (22.4) | 6 (17.1) |
| Thoracolumbar junction | 30 (61.3) | 19 (54.3) |
| Lumbar | 8 (16.3) | 10 (28.6) |
Table 3
Fracture mechanism according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification in the rigid-spine group and the non-rigid spine group
| Fracture type | Fracture number | |
|---|---|---|
| Rigid-spine group | Non-rigid-spine group | |
| A0 | 1 | 3 |
| A1 | 13 | 9 |
| A2 | 0 | 1 |
| A3 | 17 | 13 |
| A4 | 12 | 11 |
| B1 | 0 | 0 |
| B2 | 3 | 0 |
| B3 | 1 | 1 |
| C | 2 | 0 |
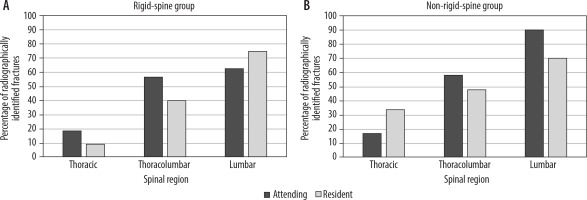
The performance of both readers and resultant diagnostic accuracies for the radiographic detection of acute TL fractures in relation to CT as the standard of reference are presented in Tables 4A, B. The performance of the attending radiologist (overall and in both subgroups) was better than the resident’s. Significantly more false positive acute fractures were reported by the resident, especially in rigid spine group (Table 4A). The missed fracture rate was higher in rigid-spine than in non-rigid-spine patients for both readers. In both groups, the percentage of unrecognised fractures was higher for the resident 61.2% (n = 30) in the rigid-spine group and 48.6% (n = 17) in the non-rigid-spine patients, compared to the attending radiologist (51.0%, n = 25 and 40.0%, n = 14, respectively). Fractures overlooked by the resident consisted of 10 stable fractures (type A0-A2) and 20 unstable fractures (16 type A3-A4 and 4 type B-C) in rigid-spine patients, and 6 stable fractures (type A0-A2) and 11 unstable fractures (10 type A3-A4 and 1 type B-C) in non-rigid-spine patients. Radiographically overlooked fractures by the attending radiologist consisted of 9 stable fractures (type A0-A2) and 16 unstable fractures (12 type A3-A4 and 4 type B-C) in rigid-spine patients, and 5 stable fractures (type A0-A2) and 9 unstable fractures (9 type A3-A4) in non-rigid-spine patients. The missed fracture rate was higher for thoracic spine than lumbar spine (Figure 1). Misclassification as chronic deformity was identified as an important factor in misdiagnosis of type A fractures (in 6 cases for the attending radiologist and in 8 for the resident). The interobserver agreement for the identification of acute fractures was found to be moderate (κ = 0.44, concordance rate 89.7%) in the rigid-spine group and substantial (κ = 0.67, concordance rate 95.1%) in the non-rigid-spine group.
Table 4A
Numbers of fractures identified on radiographs
Table 4B
Reliability of spinal radiographs for the detection of acute thoracolumbar spine fractures using computed tomography as a reference standard (%)
Discussion
The aim of this paper was to assess the diagnostic accuracy of plain films in detecting TL fractures in minor trauma patients – both with and without spinal ankylosis – using CT as the reference standard. Plain films were evaluated by a radiology resident and an experienced radiology consultant, who were blinded to the CT results. Regardless of reader experience, the sensitivity of plain films in detecting fractures was low (with the best reader achieving 49% sensitivity in the rigid-spine group and 60% in the non-rigid-spine group), resulting in a significant number of missed injuries.
Previous publications, which mostly focused on major trauma patients, have also revealed poor diagnostic accuracy of plain films, with reported sensitivities ranging from 22% to 73% [21-24]. Several studies have suggested that missed isolated fractures of the transverse process, lamina, and spinous process significantly decrease the sensitivity of plain films compared to CT [21,24,25]. Although these fractures cannot be disregarded from either a legal or clinical standpoint – because they increase morbidity and influence treatment (including analgesic and rehabilitation protocols) – the most critical issue is the rate of missed unstable fractures, which can result in serious medical consequences such as delayed paralysis [21,24,26]. In this regard, the results of previous studies are discrepant: while Hauser et al. [24] and Berry et al. [23] reported that no unstable fractures were missed by X-ray, Wintermark et al. [22] found that the sensitivity of radiographs for unstable fractures was only 33.3% – all in studies of severe trauma patients. Our results demonstrate that plain films also have poor sensitivity for detecting potentially unstable fractures in minor trauma patients. Both observers missed a significant number of acute burst fractures (types A3 and A4), with many (58.82%) being misclassified as chronic deformities (Figures 2 and 3). Fractures located in the lower thoracic spine (at T11 and T12 levels) were often overlooked on lumbar X-rays by the radiology resident (68.8% of missed type A3-A4 fractures and 60% of missed type A1 fractures) as well as by the attending radiologist (47.06% and 30%, respectively).
Figure 2
Vertebral body type A4 fracture in a 91-year-old woman who reported to the emergency department after a fall from standing height. A) Lateral radiograph of lumbar spine shows T11 vertebral body biconcave deformity with anterior cortex angulation interpreted as chronic deformity (arrow). B) Sagittal computed tomography images of lumbar spine demonstrate T11 vertebral body fracture (complete burst fracture) involving both endplates (arrowheads) and posterior wall (arrow)

Figure 3
Vertebral body type A3 fracture in an 87-year-old woman who reported to the emergency department after minor trauma. A) Lateral radiograph of lumbar spine shows loss of height in the anterior and middle parts of the T12 vertebral body interpreted as chronic deformity (arrow). B) Sagittal computed tomography images of lumbar spine demonstrate T12 vertebral body fracture (incomplete burst fracture) involving superior endplate (arrowhead) and posterior wall (arrow)

Qasem et al. [27] performed a prospective study of 136 patients with 139 acute osteoporotic vertebral fractures and found that in the first 2 weeks post-injury, 70.5% of the fractured vertebrae did not exhibit significant collapse on X-ray (an anterior vertebral height ratio > 80%). In addition, Ballock et al. [12] observed that classical radiographic signs of burst fractures – such as widening of the interpedicular distance or posterior cortical height loss – are often absent, particularly in fractures with less than 30% anterior wedging [12]. In our material, all but 5 (29.4%) of the missed burst fractures showed only minimal to mild vertebral collapse. This suggests that unstable fractures in minor trauma patients may initially present with only small deformities or displacements, rendering them difficult to diagnose on plain films. Strickland et al. [28] performed a retrospective review of lumbar spine radiographs and MRIs conducted within 30 days at a single institution and found that X-rays are unreliable for differentiating acute from chronic osteoporotic vertebral compression fractures. Their results indicated that approximately 48% of acute fractures are incorrectly classified as chronic when using radiographs alone. Conversely, Hauser et al. [24] reported that, based on plain films, 12.6% of old fractures were misclassified as acute. In our material, only 3 old fractures were misclassified as acute by the attending radiologist, while 6 acute fractures were deemed chronic. Interestingly, the resident reported significantly more falsely positive acute fractures, which, if X-ray was used to stratify patients for CT, would lead to the diagnosis of more fractures on a per-patient basis.
All type B and C fractures in rigid spine patients were also missed by both readers. Unstable fractures are common in patients with DISH and AS, and several previous publications highlighted problems with their radiographic identification (Figure 4) [13,29]. Barkay et al. [29] found that plain radiographs identified between 21% and 58% (mean 40%) of TL hyperextension fractures in patients with ASDs, depending on the observers’ experiences. Significantly fewer fractures were identified in the thoracic spine (26%) than in the lumbar spine (55%). Lantsman et al. [13] studied acute vertebral fractures in DISH patients with available radiographs and whole-body CT. In their study, the sensitivity for fracture detection on radiographs was low (47.1% for thoracic spine and 62.5% for lumbar spine), but specificity was high (96%, 95.5%). Fractures of ankylosed spine may be difficult to diagnose radiographically due to osteoporosis, ossification of the spinal ligaments, kyphotic deformity, and previous fracture [29,30]. None of the missed type B and C fractures in our material showed significant displacement. Similarly to previous reports, both readers identified significantly fewer fractures in the thoracic spine in both subgroups [13,29]. In this region, overlying rib shadows and lung structures may obscure traumatic lesions.
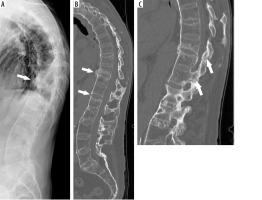
Figure 4
Overlooked multilevel hyperextension fractures in a 73-year-old man with ankylosing spondylitis after minor trauma. A) Lateral radiograph of thoracolumbar spine shows disruption of the ossified anterior longitudinal ligament at T10-T11 level (arrow) which was missed during X-ray assessment by both readers. B) Sagittal computed tomography images of thoracolumbar spine demonstrate hyperextension fractures (arrows) across the T10-T11 and T12-L1 disc spaces extending to the (C) ankylosed facet joints and a calcified supraspinous ligament (arrows)
The low diagnostic accuracy of TL spine X-rays in trauma patients necessitating CT imaging may prolong patient turnaround times and contribute to ED overcrowding. Aso-Escario et al. [31] found that 15.5% of patients with delayed diagnosis of TL spine fractures had previously presented to the ED, where only X-ray and clinical examination were performed. Missed or delayed diagnosis due to inadequate imaging can lead to inappropriate treatment, resulting in a higher incidence of neurologic injury and impacting patient outcomes, thus increasing the risk of litigation.
This study has several limitations that should be acknowledged. The retrospective design and selection criteria, which required patients to have both radiographs and CT (with only those presenting more pronounced symptoms undergoing CT) might have introduced selection bias. Additionally, the absence of a control group consisting of patients without fractures (but with both X-rays and CT) limits the assessment of the diagnostic accuracy of radiographs because it prevents a direct comparison between true positive and false positive results per patient. Unfortunately, we were unable to recruit a sufficiently large, age/sex-matched control group. Another limitation is the exclusion of orthopaedic surgeons as readers. However, previous studies have shown that orthopaedic surgeons and radiologists achieve comparable diagnostic accuracy when assessing trauma images [32].
Conclusions
This study supports the notion that plain radiographs are ineffective for diagnosing acute TL spine fractures in minor trauma patients, particularly in cases involving a rigid spine or chronic vertebral deformities. Therefore, CT should be preferred as the first-line diagnostic test. After minor trauma, vertebral deformation and displacement may be subtle, complicating accurate assessment. Special attention should be given to fractures in the lower thoracic spine when evaluating lumbar radiographs.