Introduction
Rigid spine refers to congenital or acquired ankylosis of spinal elements. Degenerative spondylosis (DS), disseminated idiopathic skeletal hyperostosis (DISH), and ankylosing spondylitis (AS) are the most common ankylosing spinal diseases (ASDs). DS is the most widespread spinal condition, with an estimated 95% of men and 70% of women over 60 years old showing at least one feature of spinal arthritis on imaging [1]. The prevalence of DISH in people over 50 years of age is estimated at 25% in men and 15% in women [2]. AS, which typically begins before age 30 years, has a significantly lower prevalence (between 0.1% and 1.4%) [3]. Before the systematic analysis by Westerveld et al. [4], the literature on fractures in rigid spines mostly consisted of case reports and series. Westerveld’s study highlighted the distinct course of spinal fractures in patients with DISH and AS [4]. These patients more often experience fractures after minor trauma, have unstable fractures, and are more likely to suffer medical complications [4]. Both DISH and AS cause long-segment spinal ankylosis, significantly altering spinal biomechanics [4,5]. In DISH, ligament ossification causes bony bridging of multiple vertebral bodies, particularly at the T7 to T11 levels [6]. In AS, inflammation promotes syndesmophyte formation and apophyseal joint ankylosis, ultimately leading to a completely ankylosed spine [7,8]. Conditions causing short-segment ankylosis supposedly have a less pronounced effect on spinal biomechanics, but this has not been studied as extensively. Reports of fractures associated with block vertebrae are scarce [9]. A concept of early DISH (pre-DISH) has been introduced to define spinal changes that fall short of meeting Resnick’s criteria; however, with time they are bound to progress to DISH [10].
To the best of our knowledge, the effect of pre-DISH on spinal susceptibility to trauma has not been investigated. Finally, despite its high prevalence, advanced DS has mostly been discussed in the context of cord injury without radiologic abnormality, rather than fracture characteristics [11].
At our tertiary referral non-trauma centre, complications from minor trauma in elderly patients are commonly encountered. Thoracolumbar fractures are prevalent in this population and are prone to being overlooked by clinicians and radiologists [12,13]. Many of these patients have rigid spine conditions. To prevent missing occult spinal fractures in this population, early-stage computed tomography (CT) scanning has been encouraged at our institution. The main purpose of this study was to assess the impact of different types of spinal ankylosis (both long- and short-segment) on the morphology and course of acute thoracolumbar fractures and, based on the results, to reevaluate the diagnostic algorithm.
Material and methods
This is a retrospective, Institutional Ethics Committee-approved study (AKBE/188/2022) of acute thoracolumbar fractures in patients admitted to the emergency department (ED) of our academic tertiary non-trauma referral centre hospital between January 2014 and December 2020. Informed patient consent was waived due to the retrospective nature of the study.
Study group identification
Patients were identified by searching CT reports for the following phrases: acute fracture, fracture, thoracic spine, lumbar spine, thoracolumbar spine.
The inclusion criteria were as follows: acute thoracolumbar fractures other than isolated spinous or transverse process fractures and available fully diagnostic CT scans. Fractures were classified as acute when diagnosed within 6 weeks of a traumatic event, provided cortical disruption or impaction of the trabeculae and/or thickening of prevertebral soft tissues were present [14].
The exclusion criteria were as follows: chronic fractures with signs of remodeling, pathological fractures, insufficiency fractures other than osteoporotic, and history of prior spine surgery.
Patients were divided into a rigid spine group with fractures involving ankylosed or adjacent non-ankylosed spinal segments (intervertebral disc and vertebra located immediately above or below the ankylosed segment) and a control group without spinal ankylosis or with fractures involving only distant non-ankylosed spinal segments.
Patients in the rigid spine group were further divided into DISH, pre-DISH, AS, DS, and block vertebrae subgroups. The diagnoses of DISH and pre-DISH were made according to Resnick and Kuperus criteria [15,16] (Table 1). All patients with AS had a pre-established diagnosis. The DS group comprised patients without features of DISH/AS, who had bridging osteophytes or facet joint ankylosis associated with loss of intervertebral disc height and facet joint osteoarthritis. Spinal ankylosis was further classified as either short (< 4 vertebrae) or long segment (≥ 4 vertebrae).
Table 1
Criteria for the diagnosis of DISH and pre-DISH (early DISH)
Data analysis
Patient characteristics: The age and sex of all patients in the rigid spine and control groups were recorded. The medical records of rigid spine patients were analysed for trauma mechanism, presenting symptoms, neurological status, and course of treatment.
Computed tomography: Due to the retrospective nature of the study, CT scanning protocols varied. However, all scans had a maximum slice thickness of 2.0 mm, were reconstructed using bone and soft tissue algorithms, and included multiplanar reformations.
Consensus reading of CT scans was performed by 2 radiologists with more than 10 years of experience in musculoskeletal radiology, who classified fractures according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) thoracolumbar classification system [17]. Furthermore, fractures were classified as single- or multilevel (contiguous and noncontiguous) and involving multiple spinal regions. As previously suggested, the following regions were distinguished: thoracic, lumbar, and thoracolumbar junction (T11 to L1) [18,19].
Statistical analysis
Statistica 13.3 software (StatSoft, Inc., Tulsa, US) was used for statistical analysis. The age of patients was described using the statistical measures mean, median, and interquartile range, because it did not match normal distribution. The control and rigid spine groups were compared using the χ2 test, and statistical significance was set at p < 0.05.
Results
Patient characteristics
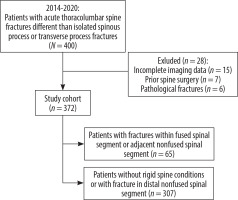
Out of 372 patients who met the inclusion criteria (Figure 1), 65 (17.47%) were placed in the rigid spine group (33 with DISH, 13 pre-DISH, 11 DS, 3 AS, 5 block vertebrae), and 307 (82.53%) in the control group (Table 2). Patients in the rigid spine group were older compared to controls: mean 78.70/64.34 years, median 81/68 years, interquartile range 9 (85-76)/32.5 (82.5-50), respectively.
Table 2
Demographic characteristics of patients in the rigid spine and control groups
All patients with DISH and AS had long-segment ankylosis. Short-segment ankylosis was present in all patients with pre-DISH (by definition), block vertebrae, and all but 2 patients with DS (one with 6-level and the other with 5-level ankylosis due to a combination of bridging osteophytes and facet joint ankylosis).
Among the rigid spine patients, 10 (15.38%) reported no recent trauma, 38 (58.46%) suffered low-energy trauma, and 17 (26.15%) reported high-energy trauma. Three patients had a GCS score of 12: one with schizophrenic psychosis and 2 with alcohol intoxication. Two patients exhibited Frankel grade D neurologic deficits, both with delayed diagnoses (by 28 and 63 days). Forty-eight rigid spine patients (72.31%) reported spinal pain at presentation (Table 3). One patient was pain-free and presented with dyspnoea. In 3 patients with GCS 12, pain location could not be established.
Table 3
Pain location in rigid spine patients
| Region | Number (%) |
|---|---|
| Spine (total) | 48 (73.85) |
| Thoracic | 4 (8.33) |
| Lumbar | 35 (72.92) |
| Thoracic and lumbar | 9 (18.75) |
| Extra spinal location | 13 (20.00) |
Of the 44 (67.69%) hospitalised patients, 25 (56.82%) underwent surgery. Eight were hospitalised for non-orthopaedic reasons, and 11 for pain management. During hospitalisation, 2 patients died of acute coronary syndrome during non-surgical stays and one from a cardiopulmonary event within one week after surgery. No patients developed new neurological deficits during hospitalisation.
CT fracture characteristics
CT was performed within 24 hours after trauma in 58 patients (92.06%). In 7 patients, the mean diagnostic delay was 21.71 days (range 3-63 days) due to minor initial pain (n = 5), pain in another region (n = 1), or an unrecognised fracture on the initial radiograph (n = 1). In 5 cases, the delay was patient related, and in 2 it was doctor related.
Overall, 607 fractures were recorded in 372 patients: 115 (18.95%) in the rigid spine group and 492 (81.05%) in the controls. Most fractures in both groups involved the thoracolumbar junction, with L1 being the most commonly affected level, followed by T12 and L2 (Figure 2).
Multilevel fractures occurred in 27 (41.54%) rigid spine patients and 93 (30.29%) controls (Table 4). A statistically significant higher incidence of single level (p = 0.039) and multilevel non-contiguous (p = 0.016) fractures were in rigid spine group compared to controls. Statistically significantly more patients with rigid spine displayed fractures in multiple spinal regions (p = 0.017). The frequency of multilevel noncontiguous fractures and fractures in multiple spinal regions was 2.1 and 1.76 times higher in the rigid spine group.
Table 4
Fracture patterns in the rigid spine and control groups
Most rigid spine fractures (46.96%) were located within the ankylosed spinal segment, while 40 (34.78%) were in an adjacent non-ankylosed segment, with the lower segment most commonly affected. All type C and all but one type B fractures were located in the mid-portion of the ankylosed segment. Additional fractures in a distant non-ankylosed segment (18.26%) were identified with a mean distance of 2.14 vertebral bodies (range 1-6) from the ankylosed segment.
Type A fractures were most common in both groups (Table 5). In rigid spine patients, 14 fractures were type B (1 B1, 6 B2, 7 B3), with 3 purely transdiscal (all B3). Only 2 rigid spine patients and 3 controls had type C fractures. Fracture types differed significantly between the rigid spine and control groups (p = 0.0015). B and C fractures were 2.53 times more frequent in the rigid spine group. Multilevel and unstable (type B and C) fractures were seen almost exclusively in patients with long-segment ankylosis, while single-level type A fractures prevailed in short-segment ankylosis patients. In 5 rigid spine patients, there was a discrepancy between spinal pain location and the fracture level on CT.
Table 5
Fracture morphology according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification
Discussion
In nearly one-fifth of the patients in our study, fractures involved an ankylosed or adjacent spinal segment. In these patients, we noted a significantly higher incidence of unstable and multilevel fractures, mainly attributable to long-segment spinal ankylosis. In the rigid spine group, all but one hyperextension fracture (type B3) were related to DISH (Figure 3), while translation injuries (type C) occurred only in AS. A single hyperextension fracture that was not DISH related was seen in a DS patient with long-segment DISH-like ankylosis, where facet joint ankylosis precluded a DISH diagnosis. These findings align with previous studies. In 2009, Westerveld et al. reviewed fractures in AS and DISH patients, revealing that most thoracolumbar fractures were hyperextension fractures (71.4% in DISH and over 93.7% in AS) [4].
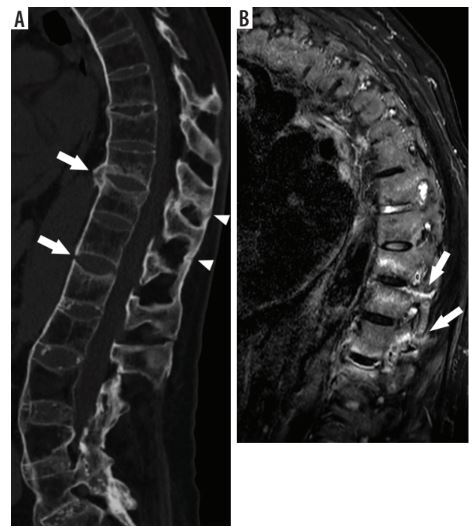
Figure 3
Hyperextension fracture in 92-year-old women with disseminated idiopathic skeletal hyperostosis after a fall from standing height. (A) Midline and (B) paramidline sagittal CT images show a transverse transvertebral distraction fracture of L1 (arrows) with preservation of the posterior spinal elements
Subsequent studies confirmed the high incidence of hyperextension fractures in AS and DISH patients and noted that type C fractures are rare in non-ankylosed spines and more associated with AS than DISH [20-25]. The tendency for unstable fractures is explained by comparing an ankylosed spine to a long lever arm transmitting stress to vertebrae at the ankylosis margins or a long bone fracturing in its midportion. Mixed results regarding the location of rigid spine fractures in previous studies suggest both theories are valid [26-29].
In our study, almost all type B and C fractures occurred in the midportion of the ankylosed segment, while compression fractures (type A) were more common at its caudal end. We observed a significantly higher proportion of type A fractures in rigid spine patients than previously reported; however, previous studies often included cases with cervical fractures, which are often purely transdiscal and, most importantly, did not include cases with short-segment ankylosis [4,20,21,30,31]. In the latter group, we found almost exclusively type A fractures. In the pre-DISH subgroup, we observed 2 type B2 fractures but no hyperextension fractures, suggesting that early DISH affects spinal mechanics differently than fully developed disease. In the remaining short-segment ankylosis patients, only type A fractures were observed. Overall, short-segment ankylosis does not seem to alter spinal mechanics sufficiently to promote complicated distraction/translation injuries.
The incidence of multilevel fractures (41.54%) in rigid spine patients in our study was substantially higher than previously reported (3.5-22.0%), even when compared to a study using whole-spine CT as a reference standard [21,31-35]. This suggests that a cohort study using cross-sectional imaging is still needed to estimate the true incidence of multilevel fractures in patients with spinal ankylosis. Multilevel fractures were more common in patients with long-segment ankylosis (Figures 4 and 5).
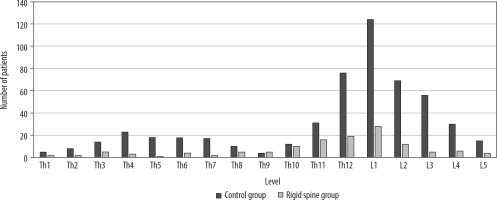
Figure 4
Hyperextension fracture in 56-year-old man with disseminated idiopathic skeletal hyperostosis after high-energy trauma. (A) Sagittal CT image shows fracture (arrow) through T8 vertebral body extending into T8-T9 intervertebral disc (discovertebral fracture) with preservation of the posterior spinal elements. (B) Coronal CT MIP image through the lumbar spine shows additional fractures of right transverse processes of L1 and L2 (arrowheads)

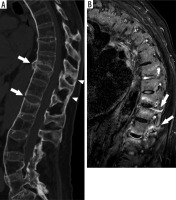
Figure 5
Multilevel noncontiguous hyperextension fractures in 73-year-old man with ankylosing spondylitis after a fall from standing height. A) Sagittal CT image of thoracolumbar spine shows hyperextension fractures (arrows) through the T10-T11 and T12-L1 disc spaces (transdiscal fractures) extending to the ankylosed facet joints and an ossified supraspinous ligament (arrowheads). (B) Sagittal STIR MRI confirms the presence of a 3-column fracture showing fractures through the ankylosed T10-T11 and T12-L1 facet joints (arrows)
The low incidence of associated spinal cord injury (SCI) in rigid spine patients in our study sharply contrasts with previous reports of SCI rates from 38% to 97% [28,36-43]. However, most earlier studies analysed cervical and thoracolumbar fractures together, with the former being a known risk factor for SCI [25,30]. In a study by Caron et al. [21], 75% of cervical fractures were associated with SCI, compared to 33% of thoracic fractures. Many previous reports were also short case series, making selection bias likely [28,39,40,42,43]. Recent studies report lower SCI rates (9.2-35.1%), but still higher than in our study [18,30,33,34]. This discrepancy is probably due to 2 factors: pre-hospital patient triage and a policy of early use of CT in older patients with spinal trauma advocated in our institution, which reduced the number of delayed diagnoses. Moreover, another spinal cord injury centre in our area receives patients with overt neurological deficits. Most patients in our study suffered minor trauma or spontaneous fractures, with neurological deficits occurring only in patients with delayed diagnoses. In a study by Balling et al. [18], neurological complications did not occur in acute low-energy injuries. Diagnosis was delayed in only 8% of rigid spine patients in our study, lower than in previous reports (19-50%) [32]. Delayed diagnosis is a known risk factor for SCI [21,30,32,44]. Caron et al. [21] observed that delayed diagnosis occurred mainly in nondisplaced fractures after trivial injuries and was associated with an 81% likelihood of neurological worsening. Reportedly, thoracolumbar fractures have higher diagnostic delay rates than cervical fractures, often progressing from neurologically intact to paralysed, especially when doctor-related delay is involved [44]. Delayed neurological deficits can occur days to months after the initial injury [30].
Our study has limitations: a moderate study group size and potential selection bias from pre-hospital patient triage. Additionally, few patients underwent magnetic resonance imaging (MRI), so the impact of this modality on treatment cannot be addressed. Nonetheless, we believe our findings and previous studies justify emphasising that among patients with rigid spine fractures, there is a subgroup of neurologically intact minor trauma patients with unstable fractures, who are at risk of delayed neurological worsening. An appropriate diagnostic algorithm is crucial to prevent complications in patients after thoracolumbar trauma; however, protocols suggested in the literature vary. There is a general agreement that hemodynamically stable patients with multiple injuries, should undergo whole-body contrast enhanced CT, which allows for the assessment of both internal organs and bones [45]. The main differences apply to minor trauma patients: US trauma protocols and recent Korean guidelines recommend using CT regardless of trauma mechanism due to the low diagnostic accuracy of plain films, while European guidelines do not preclude using radiographs as the first-line diagnostic study in stable patients without neurological deficits [45-48]. Standing radiographs are especially useful for the assessment of spinal curvatures for surgical decision-making in the early phase during patient admission or early follow-up of conservative treatment, providing more reliable estimation than supine CT [45]. The German Society for Orthopaedics and Trauma 2018 guidelines, which specifically address fractures in ASDs, recommend a 2-step diagnostic process starting with plain films and targeted CT, followed by whole-spine CT or MRI when a fracture is confirmed [49]. This approach has been criticised as time-inefficient and burdened with unnecessary radiation by Lantsman et al. [35], who recommended whole-spine CT in all DISH patients after minor trauma, except those with unspecified pain locations. They found that applying a targeted CT approach to their study group would have missed 57% of acute fractures due to discrepancies between patients’ symptoms and fracture location [35]. Our results, with a high incidence of unstable and multilevel fractures, also support long CT scans in patients with ASDs. However, in 20% of our patients, spinal complaints were masked by pain in another location (Table 3). Finally, like Katoh et al. [44], we observed that a significant number of patients reported no apparent injury episode. Therefore, we suggest at least thoracolumbar CT in neurologically intact patients with long-segment spinal ankylosis (≥ 4 vertebrae): 1) after any relevant trauma (major trauma, fall from standing height), even if the spine is painless; and 2) when the spine is painful, even if there is no trauma history. If ASD is known beforehand, plain film imaging may be omitted. In patients with short-segment ankylosis, compression fractures are most likely, and plain films should suffice for initial treatment planning in most cases.
Conclusions
We observed a significant number of unstable and multilevel fractures in neurologically intact patients with long-segment spinal ankylosis. When plain films are used as initial diagnostic test for suspected thoracolumbar trauma and long-segment spinal ankylosis (≥ 4 segment) is observed, thoracolumbar CT should be used for further evaluation.