Introduction
In recent years, a marked increase in the incidence of inflammatory bowel disease (IBD) has been observed, accompanied by prolonged patient survival. This trend has naturally led to a rise in the number of complications. Although contemporary therapeutic approaches in IBD management have significantly improved outcomes, they are not devoid of adverse effects. Some of these complications, previously unreported or exceedingly rare, may present with severe clinical manifestations, and they can be both debilitating and life-threatening [1–5].
Accordingly, the objective of this article is to highlight significant, atypical complications with severe clinical courses that should be considered in routine radiological practice.
Case reports
Case 1
A 54-year-old patient was admitted to the Department of Gastroenterology because of exacerbation of Crohn’s disease (CD) with symptoms of abdominal pain, diarrhoea, nausea, and loss of appetite. The diagnosis of CD was made 20 years earlier; at this time, due to stenosis, a partial resection of the ileum was provided, approximately 15 cm long. Until now, she has been treated with mesalazine at a dose of 2.0 g daily.
Toxins A, B and GDH antigen were detected in the stool, confirming Clostridioides difficile (C. difficile) infection. The patient was isolated and treated with vancomycin and metronidazole.
On the sixth day of hospitalisation, logical contact deteriorated. The patient was confused and presented the first in life convulsive seizure with complete loss of consciousness, without urination or defecation. During the attack, blood pressure (BP), heart rate (HR), oxygen saturation, and blood glucose levels showed no abnormalities. Wide pupils with slow reaction to the light, tendency to Babinski’s sign without focal symptoms, and negative meningeal symptoms were revealed in neurological examination.
The attacks continued in the following days, 4-2 times a day, and the patient was somnolent, unable to communicate verbally and logically. The patient was treated with diazepam and valproic acid 400 mg i.v. twice a day after neurological consultation.
Laboratory tests showed significant electrolyte disturbances: hypokalaemia, hyponatraemia, and hypochloraemia and elevated levels of C-reactive protein (CRP). To exclude neuroinfection, cerebrospinal fluid (CSF) was examined, which showed no significant abnormalities.
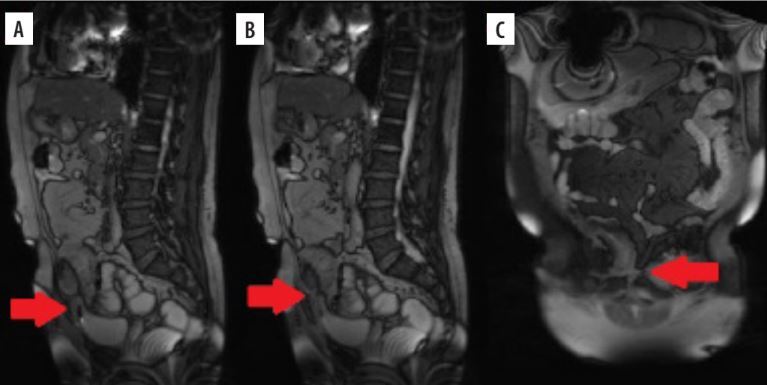
The EEG examination showed pathological and paroxysmal changes with a predominance of the left side. A head computed tomography (CT) examination showed no abnormalities, so magnetic resonance imaging (MRI) was performed, which revealed T2 and TIRM hyperintense areas in the white matter of the occipital and parietal lobes, bilaterally; the suspicion of posterior reversible encephalopathy syndrome (PRES) was proposed (Figure 1).
Figure 1
A 54-year-old woman with posterior reversible encephalopathy syndrome (PRES) secondary to treatment of Crohn’s disease. MRI FLAIR axial images. FINDINGS: hyperintense, subcortical areas in the white matter in the occipital and parietal regions bilaterally
Methylprednisolone and mannitol were introduced, and the antibiotic therapy related to C. difficile was continued.
After a few days, the patient showed both EEG and clinical improvement.
Case 2
A 21-year-old patient with history of ulcerative colitis (UC) lasting for 2 years reported pain in the chest and abdomen, shortness of breath, diarrhoea with blood, and abdominal distension. Upon admission, the patient complained mainly of crushing pain in the chest with an intensity of approximately 7/10. In physical and laboratory examinations, ECG, and ECHO no abnormalities explaining such a strong pain in the chest were revealed. Due to the patient’s psychiatric history and previous somatisation disorders, a psychological background was suspected.
In the following days, the retrosternal pain increased, reported as 10/10 in the intensity scale but again clinical, laboratory, and ECG examinations did not show any abnormalities. The patient refused to take oral medications.
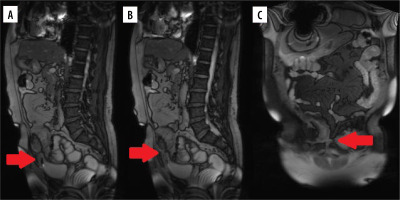
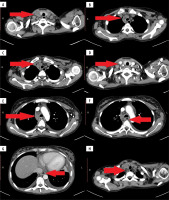
CT examination of the thorax and abdomen was performed, which revealed a widened mediastinum with inhomogeneous increase of fatty tissue density, lymph node enlargement with blurred outlines, and most importantly, the presence of small air bubbles and irregular contours in the oesophagus with slightly increased density of its walls. Oesophagitis with the presence of possible fistulas as well as mediastinitis with abscess formation was suggested. What is more, inflammatory changes of the jejunum and ileum were detected (Figure 2).
Figure 2
A 21-year-old woman with mediastinitis secondary to Crohn’s disease. Computed tomography with contrast agent administration; axial images. FINDINGS: A fluid collection with gas bubbles extending from the thyroid gland to the lower mediastinum (A, B, C, D). Enlarged mediastinum with increased density of fatty tissue and enlarged lymph nodes (E, H) as well as strengthening of the oesophageal wall (F, G)
Due to these suspicions, fluoroscopy and CT examination of the oesophagus with oral contrast administration were performed – in both studies, there was no conclusive proof of the presence of a fistula. In gastroscopic examination followed by microscopic analysis, massive inflammation of the oesophagus was diagnosed.
Due to oesophageal and small intestine involvement, based on clinical, radiological, and histopathological findings, the original diagnosis of ulcerative colitis was changed to CD.
Parenteral nutrition, antibiotic therapy (ceftriaxone, metronidazole), as well as methylprednisolone treatment were introduced together with continuity of omeprazole administration. Remission of the lesions and improvement of the clinical condition were achieved.
Case 3
A 58-year-old patient was admitted to the Department of Gastroenterology due to exacerbation of CD with symptoms of diarrhoea and pain located in the lower abdomen, mainly on the right side, lasting a week. The patient also reported pain and swelling in the scrotal area, and recurrent urinary tract infections (UTIs). Epididymitis was diagnosed, and the patient underwent antibiotic therapy.
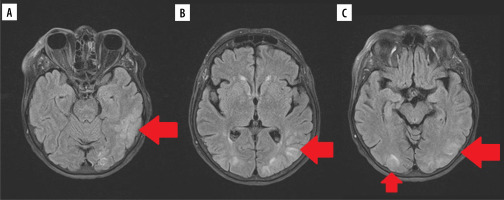
During hospitalisation, MR enterography was performed where long-term thickening of the distal ileum wall, the formation of an ileo-sigmoid fistula, and the ileo-urachal fistula were found. The intestinal content leaked into the bladder. The patient was qualified for elective surgery, during which the fistula was cut off. After the operation and completion of antibiotic therapy, the genitourinary complaints subsided (Figure 3).
Discussion
CD is a chronic relapsing IBD. It is characterised by a transmural granulomatous inflammation, which can affect any part of the gastrointestinal tract, most commonly the ileum, colon, or both. Its prevalence has continually increased over the past 50 years, with the highest incidence being reported in northern Europe and North America. Based on epidemiological, genetic, and immunological data, CD is considered to be a heterogeneous disorder with multifactorial aetiology, in which genetics and environmental factors interact to manifest the disease. The risk factors implicated with CD include smoking, low fibre, high carbohydrate diet, and altered microbiome. CD most often presents in patients younger than 30 years, although the morbidity has been increasing with age. Many studies have failed to find any sex predominance in Western countries, whereas the incidence of CD has been proven to be higher in Asian men than in women. The treatment of CD is multidirectional, so anti-inflammatory, immunosuppressive, biological, and antibiotic therapies are used together with surgery [2,6-8].
The complications of the disease are very diverse. They include intestinal symptoms as well as extraintestinal ones. The most common are the following: intestine stenosis, abscesses, fistulas, anaemia, osteoporosis/osteopaenia, peripheral arthritis with arthralgia, aphthous stomatitis, gallstones, and urolithiasis. Less frequent complications comprise ankylosing spondylitis, pyoderma gangrenosum, and ocular, like uveitis, iritis, episcleritis, keratopathy, keratoconjunctivitis, and retinal vasculitis, as well as primary sclerosing cholangitis. Apart from those mentioned above, it may manifest in rare complications related not only to the disease, but also to treatment methods [9–12].
Therefore, the aim of this study was to present 3 cases of rare complications of CD disease to deepen knowledge about disease and improve radiologists’ competences in daily clinical practice. The chosen situations are coming from the nervous, gastrointestinal, and genitourinary systems.
Case 1
PRES is a serious neurological disorder of acute or subacute onset, diagnosed mainly on the base of MRI imaging. It is potentially reversible, but if left untreated, it can even result in death [13–15].
The exact aetiopathogenesis is unknown; it is usually associated with acute or chronic hypertension, but also with acute autoimmune diseases, dyselectrolytaemia, renal failure, and sepsis. It also occurs after contact with cytotoxic drugs, immunomodulators, or monoclonal antibodies [14,16,17].
The symptoms are various and numerous; they include headache, convulsions, disturbances of consciousness or vision, nausea, vomiting, and less commonly, hemiparesis, and cerebellar or truncal syndromes. The severity of signs also varies – consciousness disorders range from mild disorientation, through agitation, to coma [13–15].
On imaging studies PRES typically manifests as white matter vasogenic oedema. It can be visible on non-contrast CT scans, but MRI T2-sequences play a leading role in establishing diagnosis due to much higher tissue resolution. MRI shows diffuse areas of increased signal in the typical location of parieto-occipital regions, which are involved in more than 90% of cases; much less often the frontal and temporal lobes, deep brain nuclei, brainstem, and spine are enclosed. The lesions are almost always bilateral, often symmetric, and subcortical. Non-typical presentations can include diffusion restriction, contrast enhancement, or haemorrhage, which are not related to vasogenic oedema [15,18-21].
Due to nonspecific features, the differential diagnosis of PRES is broad and comprises entities with confluent T2 white matter hyperintensities like ischaemia, infarction, demyelinating or infectious diseases, vasculitis, and various metabolic disorders [18,19,21].
In our case, PRES manifested as a typical, bilateral, a little bit asymmetrical, parieto-occipital pattern of vasogenic oedema with left hemisphere dominant (correlated with EEG results), which, combined with clinical symptoms, allowed us to establish a diagnosis.
Cases of PRES in the course of CD have been reported to be associated with development of sepsis or use of immunomodulatory drugs: infliximab, ustekinumab, or mesalazine. In our case, the most likely reason for PRES was an electrolyte disorder, but mesalazine treatment could aso have caused the complication [22–27]. To sum up, when the neurological condition deteriorates in IBD patients, especially during immunosuppressive or biological therapy, PRES must be considered as one of the most likely complications.
Case 2
Due to diagnostic difficulties, indeterminate colitis has been identified – this term refers to IBD cases in which the histological examinations do not allow a definite differentiation between CD and UC. In practice, patients are often diagnosed with UC, but after some time, based on clinical symptoms or imaging studies, the primary diagnosis is changed to CD, as in our case, where disease manifested as a relatively rare form of oesophagitis [28–30].
Due to the earlier diagnosis of UC and non-specific symptoms of chest pain, which could be correlated with previously diagnosed mental illness, the diagnosis of oesophagitis was delayed, which most likely resulted in a severe complication in the form of mediastinitis.
An oesophageal CD can lead uncommonly to fistulous formation between the digestive tube and tracheobronchial tree or mediastinum causing pneumonias, paraoesophageal abscesses, and general inflammation of mediastinal structures. Searching the PubMed database, we found only 2 cases of mediastinitis in the course of CD – in each there was the presence of a fistula [31,32].
A routine chest X-ray radiograph can reveal features of mediastinitis like widening of the middle shadow, changes of the right paratracheal lane, emphysema, subcutaneous emphysema, or pleural effusions, but the diagnostic quality of this technique in terms of sensitivity and specificity is very low. Therefore, CT stands as a gold standard diagnostic method when the slightest suspicion of acute mediastinitis arises [29,30]. CT enables the detection of all the findings mentioned above but also even small fluid collections, gas bubbles, increased attenuation of fat, enlarged lymph nodes, as well as others related to the specific aetiology [33–35].
Because in our case, radiological examinations with oral contrast administration did not confirm the presence of a fistula, most likely due to its small size, conservative treatment was provided.
Case 3
The urachus is a fibrous remnant of the allantois, a canal that drains the urinary bladder of the foetus that runs within the umbilical cord. Patent urachus belongs to the spectrum of rare anomalies that result from failure of involution of the embryologic tissues. Maintaining patency in adult life may lead to several developmental abnormalities such as the following: urachal cysts, umbilical fissures or full fistulas, and tumours of this structure. Urachal anomalies are usually the source of nonspecific clinical symptoms, typically mimicking other abdominal or pelvic pathological processes [36,37].
Creation of fistulas is a common complication of CD, especially between adjacent bowel loops, or between the bowel and bladder or vagina. Among all fistulas to the urinary system in CD, entero-vesical ones represent 8-12% of them, while entero-uracho-cutaneous 0.6-1% only [38].
They manifest clinically as pneumaturia, dysuria, UTIs, fecaluria, haematuria, and urorrhea. They can also be asymptomatic [38]. In our case, the fistula was formed between the ileum and the urethra, which created the possibility of passing intestinal contents into the bladder, and thus – most likely – recurrent urinary tract infections and orchitis.
MRI is a method of choice in evaluating fistulas. They are visible as an abnormal tubular connection between 2 organs, vessels, or tissues with preserved lumen. Sometimes it is impossible to detect fistulas directly due to technical limitations of imaging or the fact that fistulas can open and close. Then indirect signs like the presence of gas bubbles in the urinary bladder coming from to the gastrointestinal tract establish diagnosis [37,39,40].
Conclusions
Complications of CD and its treatment can occur in various organs and systems and manifest in very non-specific ways. If unnoticed, they even be life-threatening; therefore, it is important in clinical practice to take into account the possibility of their presence when evaluating patients with CD.