Introduction
In recent years, the healthcare community has faced unprecedented challenges, including the coronavirus disease 2019 (COVID-19) pandemic, increasing demand for medical imaging, and a growing shortage of radiologists [1,2]. These pressures have accelerated the development and adoption of artificial intelligence (AI) in medical imaging, aiming to improve efficiency and accuracy in tasks like classification, segmentation, detection, and clinical decision-making [3-5].
Numerous studies have applied AI systems to chest computed tomography (CT) [6-8], but many primarily focused on evaluating their technical and clinical feasibility, often limiting their analysis to stand-alone performance metrics [9]. Although some researchers have compared these models directly to the performance of radiologists [10,11], relatively few have investigated their influence on what is termed “diagnostic thinking efficacy” [12,13]. This concept extends beyond diagnostic accuracy to evaluate the added value AI brings to the diagnostic process, including its capacity to enhance radiological decisionmaking and impact clinical judgment [14]. Importantly, the integration of AI systems into clinical practice does not automatically translate into improved decision-making. Receiving AI-generated results can trigger complex cognitive processes in radiologists, involving confirmation or disconfirmation of their initial judgments, which may affect the final diagnostic outcomes [15].
As learned from the COVID-19 pandemic, distinguishing between different types of viral pneumonia serves as a prime example of a challenging classification task. Typical CT characteristics have been identified for various infectious agents, but significant overlap in findings reduces their specificity and complicates accurate diagnosis, especially in high-pressure clinical scenarios [16-19]. In this context, Meng et al. [12] recently demonstrated the benefits of AI-human interaction in improving diagnostic accuracy and confidence when distinguishing between COVID-19 and community-acquired pneumonia. However, they focused solely on the effect of presenting AI results before individual diagnosis, without addressing how different AI usage strategies might variably affect radiologists’ performance.
Building on this foundation, our study investigates the impact of integrating an AI classifier into the complex diagnostic process of distinguishing between viral pneumonias. Specifically, we assessed how AI integration influenced diagnostic accuracy and decision-making efficiency, using the COVID-19 Reporting and Data System (CO-RADS) as a structured framework [20]. Furthermore, we compared two distinct AI usage strategies to determine the optimal approach: a “default approach”, where AI outputs were available for all cases, and a “selective approach”, where AI support was limited to equivocal cases. Our aim was to evaluate not only how diagnostic performance varies across these different strategies but also their different potential to reduce uncertainty and build trust in AI-assisted workflows.
Material and methods
Study design and imaging data
This study received approval from the Local Ethics Committee, and informed consent was waived because data were collected retrospectively and processed anonymously.
The analysis was performed on a random cohort of 220 patients with respiratory symptoms who underwent a CT scan within 15 days of serological evidence of infection from either SARS-CoV-2 (COVID-19, n = 151) or other respiratory viruses (non-COVID-19, n = 69). The CT scans of COVID-19 patients were acquired between March 2020 and April 2021, during the pandemic, while scans of non-COVID-19 patients were performed between January 2015 and October 2019, prior to the emergence of COVID-19. The inclusion of temporally distinct cohorts was essential to avoid misclassification between different viral pneumonia because all control cases were selected prior to the emergence of SARS-CoV-2.
The selected sample size enabled the detection of a minimum accuracy difference of 10%, with a minimum value of 80%, while maintaining a statistical power of 80% [21]. The proportion of COVID-19 to non-COVID-19 cases was chosen to simulate a pandemic-like scenario, with a higher prevalence of COVID-19 cases, to appropriately frame the reader evaluation task, as explained below.
Chest CT examinations were acquired using various CT scanners (Siemens SOMATOM Definition Edge, Siemens SOMATOM Sensation 64, Philips Brilliance) with the patients in supine position with arms over the head for a single breath-hold, in keeping with their compliance.
The acquisition parameters were as follows: tube voltage = 80-140 kV; automatic tube current modulation; pitch = 1; matrix = 512 × 512. All acquisitions were reconstructed with high-resolution thoracic kernels and a slice thickness of 1 mm.
Reader evaluation
Three radiologists with > 10-year experience (Readers 1-3) were enrolled to evaluate the 220 CT scans. The readers were blinded to the original radiologic report and all non-imaging data, including the acquisition date of the CT scans and serologic findings. They were asked to assign each case a CO-RADS score (1 to 5) to indicate the level of suspicion for COVID-19, both before (S1) and after (S2) being provided with an AI-generated probability (0-100%) that the CT scan belonged to a COVID-19 patient. The CO-RADS scoring system is an established framework used to evaluate the likelihood of COVID-19 based on CT imaging findings. Scores of 1 and 2 suggest a diagnosis other than COVID-19, a score of 3 is designated for equivocal cases with indeterminate findings, while scores of 4 and 5 indicate a high or very high suspicion of COVID-19. Before the test, the readers were informed that the AI classifier, based on a multi-layer perceptron architecture [22], had been previously trained and validated on a large cohort of patients, achieving an accuracy of 79% (95% CI: 73-84%) in distinguishing between viral pneumonias during the COVID-19 pandemic [23]. To simulate a comparable clinical scenario, readers were instructed to interpret the CT findings as if the patients were presenting with acute symptoms (e.g. arriving at an Emergency Department).
The test was conducted using a JavaScript-based program [24], which presented the anonymized CT series in a randomized sequence. During the first evaluation (S1), readers assigned an initial CO-RADS score using a dialogue box. The program then provided the AI-generated probability indicating whether the CT scan was likely to represent a COVID-19 case. Subsequently, the program reopened the same patient’s CT scan for a second evaluation (S2), allowing readers to either confirm or adjust their initial CO-RADS score through the dialogue box. After completing the evaluation for each patient, the program automatically loaded the next anonymised CT scan. The system recorded all assigned CO-RADS scores and the time taken by readers to analyse each CT scan during both S1 and S2 phases.
Data analysis
Continuous variables were reported as median values with 1st-3rd quartiles (Q1-Q3) of their distribution; categorical variables were expressed as counts and percentages, with corresponding 95% confidence interval (95% CI) using the Wilson method [25].
The chance-corrected inter-reader agreement for the assigned CO-RADS score was tested using Gwet’s second-order agreement coefficient (AC2) with ordinal weights [26]. AC2 was chosen to correct for the partial agreement occurring when comparing ordinal variables with multiple readers and because it is less affected by prevalence and marginal distribution [27-29]. The level of agreement was interpreted following Altman’s guidelines [30].
Sensitivity (SE), specificity (SP), accuracy (ACC), positive likelihood ratio (PLR), and negative likelihood ratio (NLR) of human readers in discriminating COVID-19 patients from non-COVID-19 patients were calculated for both S1 and S2. For the latter, two scenarios were examined: one with AI output available for all cases (default approach), and another simulating AI application exclusively to CO-RADS = 3 cases from S1 (selective approach). Performance metrics were computed for each radiologist and as an average among all readers.
The Mann-Whitney test was employed to assess the null hypothesis that readers’ evaluation time for S1 and S2 under both default and selective approaches originate from the same distribution. Significant differences in diagnostic performance among these scenarios were assessed using the χ2 test with post hoc analysis of adjusted residuals [31].
The data analysis was performed using the Real Statistics Resource Pack software (Release 6.8) (www.real-statistics.com) for Microsoft Excel (Microsoft Corporation, Redmond, Washington, USA) and GraphPad Prism 9.5.1 (GraphPad Software, La Jolla, CA).
Statistical significance was established at the p < 0.050 level.
Results
The demographic characteristics of the patient population are reported in Table 1. Out of the 220 patients, 159 (72%) were males and 61 (28%) females, with a median age of 68 years (Q1-Q3: 59-78 years). The median interval between CT scans and molecular swabs was of 1 day (Q1-Q3: 0-2 days) for COVID-19 and 3 days (Q1-Q3: 1-6 days) for non-COVID-19 patients.
Table 1
Demographic characteristics of the study population
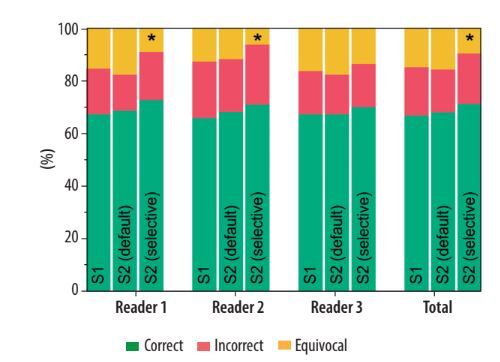
In S1, the median time required for radiologists to distinguish between COVID-19 and non-COVID-19 pneumonia cases was 10 s (Q1-Q3: 7-14 s). When AI results were introduced in S2 with the default approach, the median evaluation time increased slightly but significantly to 14 s (Q1-Q3: 10-19 s, p < 0.001). For cases where readers altered their evaluations, the median additional time compared to S1 was 4 s (Q1-Q3: 3-9 s). In S2 with the selective approach, the median evaluation time remained at 10 s (Q1-Q3: 7-15 s), showing no significant difference from S1 (p = 0.262). Evaluation time distributions are illustrated in Figure 1.
Figure 1
Distribution of readers’ chest computed tomography evaluation times in S1 and S2 under default and selective approaches
The CO-RADS scores assigned by each reader in S1 and in S2, considering both the default and selective approaches, are presented in Table 2.
Table 2
COVID-19 Reporting and Data System (CO-RADS) scores assigned to COVID-19 and non-COVID-19 patients by the readers
The inter-reader agreement for assigning the CO-RADS score was good-to-excellent across all scenarios. Specifically, in S1, the ordinal-weighted AC2 was 0.77 (95% CI: 0.73-0.81; p < 0.001), in S2 with the default approach it was 0.81 (95% CI: 0.78-0.85; p < 0.001), and in S2 with the selective approach it was 0.79 (95% CI: 0.76-0.83; p < 0.001). Perfect agreement was obtained between the 3 readers in 73/220 (33%) cases in S1, 91/220 (41%) cases in S2 with the default approach, and 82/220 (37%) cases in S2 with the selective approach. For all the evaluations, the category with the highest level of perfect agreement between the readers was the CO-RADS = 2 (range: 58-63%).
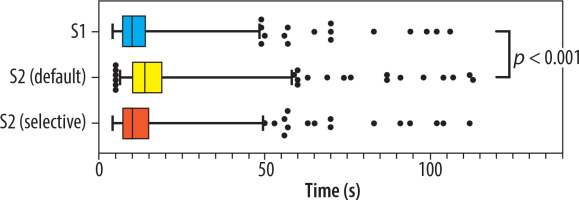
Upon reviewing the AI output in S2 with default approach, Reader 1 modified the CO-RADS score in 47/220 cases (21%), Reader 2 in 54/220 cases (25%), and Reader 3 in 16/220 cases (7%). From a clinical perspective, these changes in CO-RADS scores translated into an actual shift in classification between COVID-19, non-COVID-19, or equivocal case in 35/220 (16%) for Reader 1, 26/220 (12%) for Reader 2, and 15/220 (7%) for Reader 3. Notably, when the radiologists were confident in S1 diagnosis (i.e. CO-RADS ≠ 3), a classification change in S2 occurred in 7% of cases, on average. This prevented an incorrect diagnosis in 45% of cases, but in the remaining 55% a correct classification was missed. When considering only the score variations when a CO-RADS = 3 was initially assigned, corresponding to the selective approach, changes were observed in 14/220 (6%) for Reader 1, 14/220 (6%) for Reader 2, and 6/220 (3%) cases for Reader 3. In such a setting, the radiologists moved from an uncertain diagnosis (i.e. CO-RADS = 3) to a correct classification in 85% of the cases, on average. Some relevant examples are shown in Figure 2.
Figure 2
Representative cases illustrating different outcomes in the classification of respiratory viral pneumonias with the aid of an artificial intelligence (AI)-based classifier. For each case, the radiologist-assigned COVID-19 Reporting and Data System (CO-RADS) score is reported before (S1) and after (S2) reviewing the AI-generated COVID-19 probability. In cases where initial uncertainty (S1) was present, AI support often helped resolve the doubt. Conversely, in initially confident assessments, AI input occasionally introduced new uncertainty. The examples shown include pneumonias caused by (A) rhinovirus, (B) human coronavirus NL63 (HCoV-NL63), (C) parainfluenza virus type 3 (PIV3), and (D-F) SARS-CoV-2 infection
Regarding the diagnostic performance in identifying COVID-19 pneumonia, detailed results are provided in Table 3. Also, Figure 3 and Figure 4 provide a visual, quantitative comparison of the accuracy results between readers and different AI usage approaches.
Table 3
Diagnostic performance of the readers in classifying the patients before (S1) and after (S2) being provided with the results of the artificial intelligence classifier, under both the default and selective approaches
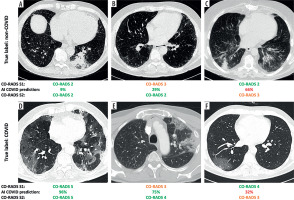
Figure 3
Confusion matrices of the global performance of the 3 readers before (S1) and after (S2) receiving the artificial intelligence classifier results, under both the default and selective approaches
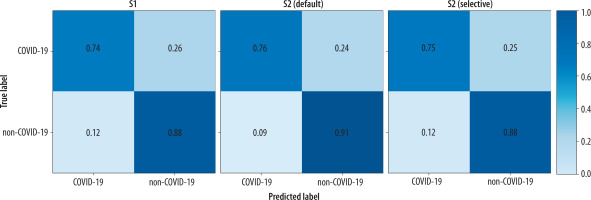
Figure 4
Comparison between the accuracy of the 3 readers before (S1) and after (S2) receiving the artificial intelligence classifier results, under both the default and selective approaches
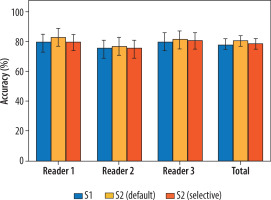
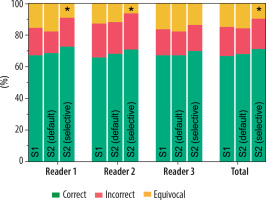
Considering all the readers, SE = 74% (95% CI: 70-79%), SP = 88% (95% CI: 82-92%), ACC = 78% (95% CI: 75-82%), PLR = 5.95 (95% CI: (4.01-8.83), and NLR = 0.29 (95% CI: 0.25-0.35) were observed in S1, with 15% of cases assigned a CO-RADS = 3. In S2 with the default approach, SE = 76% (95% CI: 71-80%), SP = 91% (95% CI: 86-95%), ACC = 81% (95% CI: 77-84%), PLR = 8.85 (95% CI: 5.44-14.40), and NLR = 0.26 (95% CI: 0.22-0.32) were globally obtained, with 16% of cases assigned a CO-RADS = 3. On the other hand, in S2 with the selective approach, SE = 75% (95% CI: 70-79%), SP = 88% (95% CI: 83-92%), ACC = 79% (95% CI: 75-82%), PLR = 6.28 (95% CI: 4.23-9.34), and NLR = 0.29 (95% CI: 0.24-0.42) were observed, with 10% of cases assigned a CO-RADS = 3. These differences in the proportions of correctly classified, incorrectly classified, and equivocal cases were not statistically significant, except when applying AI results to CO-RADS = 3 cases in the selective approach in S2. Specifically, the number of cases classified as equivocal significantly decreased compared to S1 and S2 with the default AI approach, affecting both the global performance and the individual performance of 2 out of 3 readers. Notably, no statistically significant differences were observed in the ratios of correctly and incorrectly classified cases across the different scenarios. Full details are reported in Table 4 and Figure 5.
Table 4
Distribution of correct, incorrect, and equivocal cases among the readers before (S1) and after (S2) being provided with the results of the artificial intelligence classifier, under both the default and selective approaches. The p-values from χ2 test with post hoc analysis of adjusted residuals were reported for each class (significant values are reported in bold)
Figure 5
Comparison of the distribution of correct, incorrect, and equivocal cases among the 3 readers before (S1) and after (S2) receiving the artificial intelligence classifier results, under both the default and selective approaches. The asterisks indicate classes that show significant differences from the others (p < 0.009)
Discussion
In this study, we examined how the performance of radiologists was affected when they received an independent classification from an AI-driven algorithm, focusing on a complex diagnostic task such as the differential diagnosis between viral pneumonias. Additionally, we simulated two usage scenarios: one where the AI tool was available to the readers by default for all cases, and another where AI was selectively applied to cases classified as equivocal.
A good-to-excellent inter-reader agreement (AC2 range: 0.77-0.81) in assigning the CO-RADS score was found in all scenarios. Notably, in S2, there was an increase in the rate of perfect concordance among the radiologists, although the overall effect on inter-reader agreement was limited.
In terms of evaluation time, we observed that the introduction of AI output did not result in substantial delays in the radiological assessment. The default approach added a statistically significant but highly marginal amount of time to the overall process, even when the AI prompted the readers to adjust their scores. Conversely, no significant differences were observed for the selective approach compared to the evaluation without AI.
Interestingly, AI support did not lead to significant differences in the proportions of correctly and incorrectly classified cases, with all readers achieving very similar accuracy levels across the different scenarios. Previous studies have reported AI models achieving accuracy rates ranging from 80% to over 95% in distinguishing between different types of viral pneumonia [32-36]. However, these studies most often concentrated on assessing AI performance itself rather than evaluating how effectively it integrates into the decision-making process of radiologists [14]. Furthermore, the abovementioned results may be attributed to the use of CT datasets encompassing heterogeneous pulmonary conditions, including bacterial infections [10], whose distinct features can ease the classification task.
Meng et al. [12], who analysed a well-balanced CT dataset, considering the stage and severity of pneumonia, reported an accuracy level of around 80%, closely aligned with our observations. Differently from our findings, they noted a statistically significant increase in accuracy when incorporating the AI results, but this improvement was relatively slight (less than 3%). Indeed, examining the performance of individual readers in their study, some showed no significant benefit from AI support, regardless of their experience level. Our study yielded similar results, but we also provided full details about the readers’ scores and how they changed after receiving AI output. This analysis revealed that clinically meaningful classification changes occurred in 7% to 16% of cases, revealing a fluctuating impact of AI on radiologists. Despite the varying rates of classification changes, the lack of significant performance differences among the readers can be traced back to the score adjustments made when the radiologists were initially confident in their evaluation. This introduced an element of randomness into the final performance, as AI advice prevented an incorrect diagnosis in nearly half of these cases but also led to missing the correct classification in the remaining patients.
Regarding equivocal cases, we confirmed that the AI support reduced the classification uncertainty as reported by Meng et al. [12], but only if applied when the radiologist was initially unsure about the diagnosis. In such instances, we achieved a nearly 40% reduction in equivocal cases while maintaining the same level of accuracy. Notably, we determined the confidence level not through self-assessment but by employing the CO-RADS score, thereby providing a more standardised scoring framework.
In previous research [24], we highlighted the potential of AI in assisting radiologists with the classification of equivocal cases, where the accuracy of human readers typically declines. The findings of the current study reinforce this insight, demonstrating that the selective application of AI yields the most significant benefit compared to a default approach applied to all cases. By restricting AI use to equivocal cases, this strategy minimises the risk of introducing new diagnostic uncertainties when radiologists are already confident in their initial assessments. Moreover, selective AI usage aligns with the principles of trustworthy AI by providing targeted, context-specific support, thereby enhancing diagnostic efficacy without overwhelming clinicians with superfluous information. These results highlight the value of integrating AI as an “on-demand” tool in clinical workflows, designed to assist radiologists specifically in situations of diagnostic uncertainty. This approach aligns with the recommendations of Fügener et al. [37], who emphasised that the most effective collaboration between AI and human expertise occurs when classification tasks are delegated to the actor best equipped to address them on a case-by-case basis. However, their study also revealed that overconfidence among users often hinders effective delegation to AI. By linking the decision to utilise AI with a predefined equivocal class (such as CO-RADS = 3 cases), this bias can be mitigated, ensuring AI is used effectively to support decision-making while maintaining radiologists’ autonomy and confidence in the diagnostic process. Therefore, we believe our findings contribute to the broader goal of developing strategies for trustworthy AI integration into clinical practice, supporting radiologists in complex diagnostic scenarios while enhancing confidence in, and reliability of, AI-assisted workflows.
Our study has some limitations. Firstly, all participating radiologists had extensive exposure to CT imaging of COVID-19 patients during the pandemic. It is possible that less experienced readers would have derived more substantial benefit from the AI assistance, resulting in a greater performance improvement. Additionally, the retrospective design of the study, conducted within a single institution, may have introduced selection bias. For instance, the CT scans included in our study were acquired over several years, even though no substantial changes occurred in local imaging protocols during this period. All examinations were performed using standardised chest CT protocols routinely adopted in clinical practice, including consistent acquisition parameters and reconstruction settings. Moreover, readers were fully blinded to acquisition dates and scanner details, further minimising any influence of temporal factors on diagnostic performance.
Lastly, given the reduced impact of COVID-19 on healthcare systems, the significance of these findings might seem diminished. However, the landscape could swiftly shift with the emergence of new SARS-CoV-2 variants of concern or the outbreak of other rapidly spreading respiratory viruses [38]. Moreover, our focus on viral pneumonias served dual purposes: leveraging existing knowledge and resources, including a validated AI model, while also providing a representative example of a complex diagnostic challenge in chest CT imaging. Importantly, the insights gained from understanding how radiologists interact with AI in this demanding classification task can extend beyond viral pneumonias to other domains, such as non-infectious interstitial lung diseases. Regardless of the specific application, it is crucial to recognize that even the most advanced AI systems with exceptional diagnostic capabilities will not achieve successful adoption unless they enhance diagnostic thinking efficacy and improve clinical decision-making processes. In other words, this underscores the importance of going beyond stand-alone performance metrics to identify the most effective patterns of AI usage within clinical workflows. By developing tailored strategies for AI integration that address specific contexts and minimise potential errors, we can maximise its benefits and build greater trust and confidence in its application.
Conclusions
Our study showed that AI can effectively reduce uncertainty when distinguishing equivocal cases of viral pneumonias on CT imaging. However, its reliability decreases when radiologists are already confident in their diagnoses. By adopting a selective approach that limits AI analysis to equivocal cases, radiologists can maintain comparable diagnostic accuracy while avoiding exposure to additional and potentially misleading AI-generated information to review.